More thoughts on “do you need a doc at your startup”
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
This episode of Out-Of-Pocket is brought to you by…

Medicaid enrollment is where policy meets real-world friction — a challenge that the OBBBA will intensify.
Patients often identify coverage needs when a bill arrives. And that’s where Cedar and Fortuna come in.
Fortuna modernizes Medicaid and financial aid enrollment and renewal, while Cedar delivers these resources when patients need them most.
The result? More patients covered, lower uncompensated care, and providers stay ahead of policy shifts.
It’s all part of Cedar Cover, a proactive digital safety net of affordability solutions.
–
Wanna chat about sponsorship of OOP events, newsletter, etc.? Let’s chat
Fight me you cowards
Last time I wrote out my thoughts on when it made sense to actually have a clinical leader at your startup. We went through company types where it’s a nice to have but not necessary, times where you can get away with a fractional relationship, and times where you should really have someone full time from the beginning.
I was expecting more pushback, but everyone was very respectful. I wanted some Jerry Springer style drama in the inbox, so I was disappointed. But people raised some interesting points related to the topic that I wanted to share below. I don’t necessarily agree with all of them, but they’re worth highlighting!
Memes, graphs, and commentary are by me.
—
Clinical Expertise is Not Clinical Ops
“A huge learning we had was that Clinical expertise does NOT equal Clinic Operations expertise and, in our case we have needed both. The need for each, respectively, has flexed up and down over time.
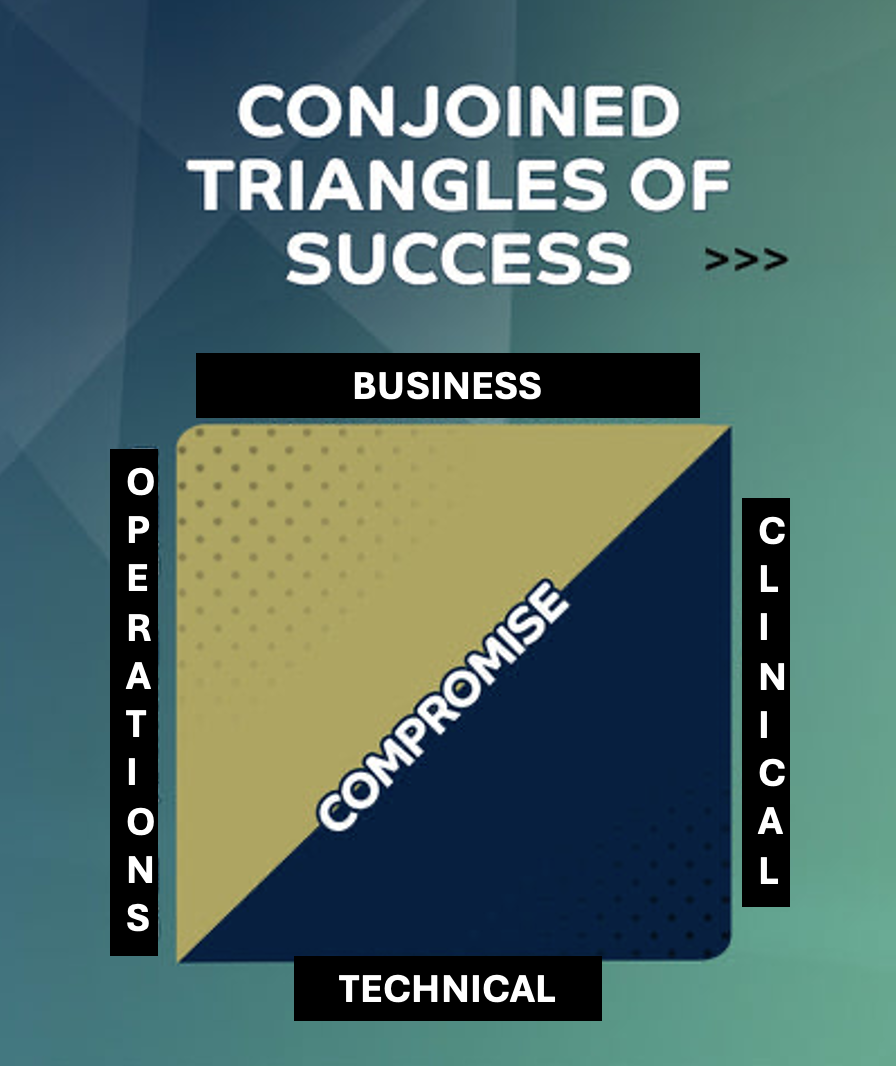
We mistakenly believed that the golden shape of a digital health startup was a triangle - Clinical, Technical, and Business. What we learned is that you need a square - add Clinic Operations as another point and boom now you’ve got a full leadership team.
At the start, we were OK without the Ops because the Clinical value was seen as high enough to deal with the operational issues faced by our early adopters. And I had enough manufacturing operations background to somewhat lessen the pain we were causing.
But once we started scaling our lack of clinical ops expertise became more and more painful and obvious. And once we brought on our Chief Outcomes Officer (started and sold her own practice, also ran dozens of clinics for a PE backed roll up) we saw the value immediately.
So, if you’re selling to a provider group and think you only need a clinical brain, you’re right, until you’re not. And that learning is tough!”
[NK note: Can’t emphasize enough how different of a skillset clinical operations is. Whenever we do our Ops Knowledgefest conference, it’s always one of the most attended sessions because every company is trying to figure out staffing, matching supply and demand, incentive structures for teams, etc.]
—
Quick announcements - Boston Healthcare Coworking!!! Healthcare 101 is Back!!
We’re excited to announce that we’re making a healthcare coworking space in Boston!! If you’re interested please fill out this form.

This means we now officially have healthcare coworking spaces going in SF, NY, Boston, and Chicago! If you want to join any of the others, you can find more details here.
With everyone in remote jobs, we’ve found that people just want to be able to sit next to other people so they can say things like “RAF” and feel something when they get a response.
Separately a reminder we have a few courses enrolling!!!
- AI products evaluation 101 (FREE, starts 10/28) - We’re partnering with Canvas to understand how to evaluate the performance and claims AI startups are making.
- Claims 101 (not free, starts 11/10) - Final run of our beloved claims course, where we teach you the basics of what’s in claims data, how to actually analyze it, and more.
- Value-Based Care 202 (FREE, starts 11/18) - We’re partnering with Navina to talk about how the practical parts of value-based care work and interesting ways AI is changing that.
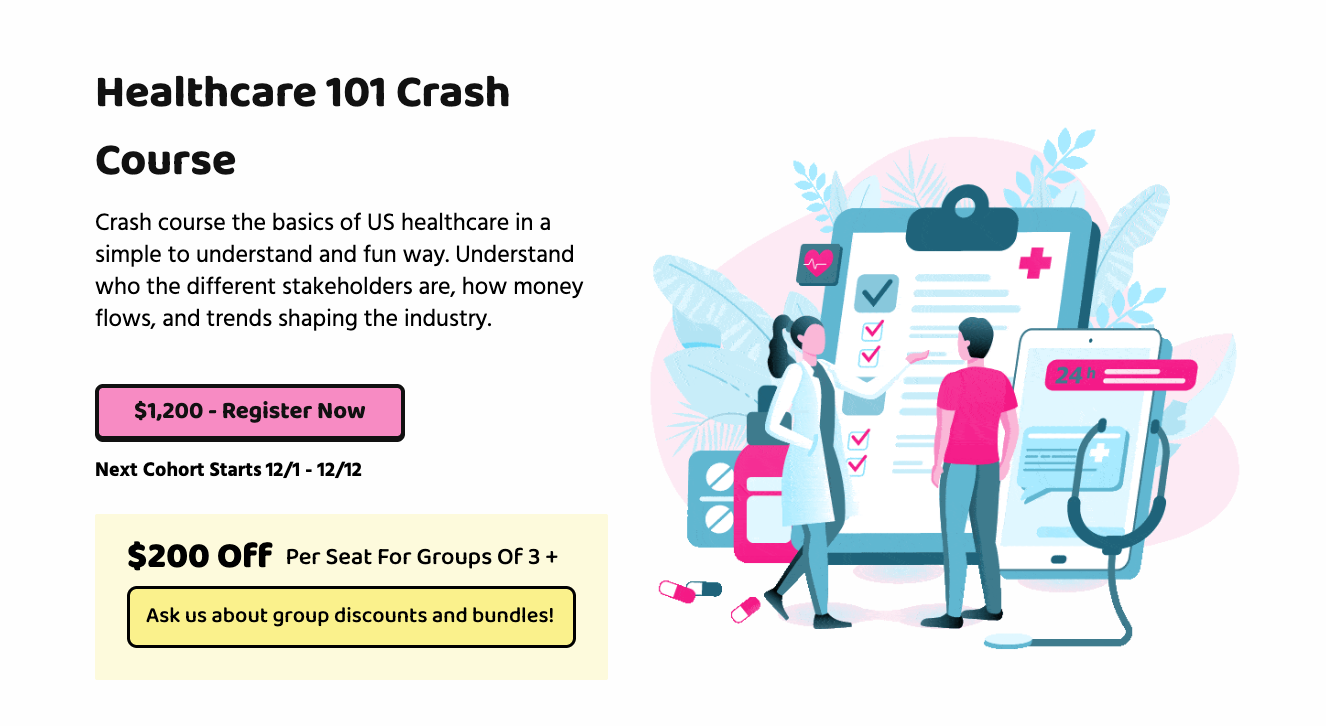
- Healthcare 101 (not free, starts 12/1) - The one, the only, Nikhil Krishnan will take you through the wild world of US healthcare. You’ll learn the jargon, understand how the money flows, and how all of these different stakeholders interact with each other. I’ll get you up to speed in how US healthcare works in 2 weeks.
We’re doing more workshops, custom courses, and group discounts so hit us up if you need to get a team up to speed.
Upskilling Physicians
“I think you captured the nuance here really well! As an MD trying to find my way in this space, I also wonder how to provide real value (and also not get bored) working at companies. In addition to seeing patients, I can understand data, advise on analytics, help ask process questions (we do a lot of hospital QA projects), advise on long-term vision, etc. If companies are going to pay for an MD, they should make sure they have concrete ideas for how that person can be most useful. Sometimes that means recognizing that they may have skills from research or training that are useful to the org even if they're not clinically relevant.
Your point about hiring a physician and then upskilling them is also well taken. This is a lot of what pharma and biotech do - they have to teach physicians how to "do" drug development, because their clinical experience from running trials is often not enough to understand the business. But once physicians understand that side of pharma, they are often well-poised to move into positions where they can advise on strategy, business development, etc. instead of just running trials.”
-Anonymous
[NK note: Remember clinicians love being in school. Just tell them upskilling is like paid school.
Btw this is where clinical advisors can be very helpful in understanding the kinds of tasks you need a doc to do at your company.]

—
1099 docs vs. Part time vs. Full time
“I think a negative consequence of all these healthcare businesses operating outside the "traditional landscape" (e.g., Ro, Hims/Hers) is that they've created a market that's become a race to the bottom with 1099 physicians functioning as "click factories" — just cogs in a larger wheel. Based on my experience, the going rate for these physicians is about $120/hour, which is incredibly cheap when you think about it. There's a whole swath of physicians being used for nothing more than their license.
Additionally, when building out my current company, I initially thought I would need to hire a full-time doctor at $350-400k/year all-in. However, I quickly realized I could work with a part-time medical director at only 20-25% time (with corresponding cost reduction), which really lowered the startup capital needed to get the business off the ground in a CPOM [Corporate Practice of Medicine] structure."
Also, never give out equity to providers in exchange for "providing their domain expertise." There's a huge disconnect between the value they perceive they bring to the organization/startup and what they actually deliver. I use this as a quick litmus test for whether to continue conversations with them.”
[NK note: Because we’re in a physician shortage in the US, a lot of docs are getting CRAZY offers (like $1M for radiologists!). Hospitals NEED these docs to deliver services, keep certain designations they have, etc. so they have to bid up compensation. I think hospital salaries often distort a lot of the comp:value conversations doctors have with startups, similar to how Google comp distorts engineers.
Also for what it’s worth, I think there’s a lot of simple health needs where it’s fine to have really lightweight interactions between a doc/patient that amount to cheaper care.]

—
Various takes about MDs
“1. An MD degree means just that. All clinicians vary, from the ones that did med school and then went to Wharton/McKinsey, through to ones who have deep clinical knowledge and are widely respected in their field.
2. Start ups are not for most MDs. They cannot handle not being the boss or listened to; their EI is not great. Further many have trouble managing the clinical/academic side with executing on commercial goals.
3. MDs that have industry experience, through commercially sponsored research. KOL roles, or innovators themselves are a rich hire.
4. MDs with academic leadership experience have an approach to develop a thesis and then build a team to execute. This is valuable at a start-up.
5. MDs with an Ivy League MBA are pretty vanilla.
6. MDs in private practice are pretty innovative, though not respected by the AMC crowd.
7. MDs generally don’t understand equity, fundraising or exits.
Finally I fully agree that more physicians should just get on with it and become founders.”
[NK note: In general, more people should understand how a business runs. How does money come in and where does it go out, how do you sell, what are tradeoffs you make when you make certain kinds of deals. Clinicians in particular are getting farther away from that as less and less of them work/run private practices.
The other day I had a doc ask ME how do practices know which insurances to take, which left a 3 second pause as I tried to figure out how we got to this point both in society and in the conversation.]
–
MDs vs. People with lived experience
“The debate isn’t whether clinical leaders matter—they do. The real question is why they’re treated as sacred early hires even when the product is built for patients and everyday consumers, not providers. Women make most healthcare decisions in this country—seeking care, paying for it, and caregiving—yet their perspectives are still missing in many health tech leadership teams.
Until we balance clinical expertise with consumer insight, we’re building for only half the reality. Many years ago I remember asking in a leadership debate around scheduling care whether anyone in the room had scheduled care for anyone besides themselves in the past year. No one raised their hand. I'd love to see a debate on filling that gap first.”
-Anjali Jameson
[NK note: My mom definitely made the healthcare decisions in our house growing up. In my house it’s a fight, because my wife just wants to schedule the appointment and I want to search the price transparency files to compare this doc against others.
Btw this is why it’s good to do focus groups and user interviews properly. You need to ask the right questions to figure out who the decision makers are, how the decisions get made, at what point in the journey, etc.]
–
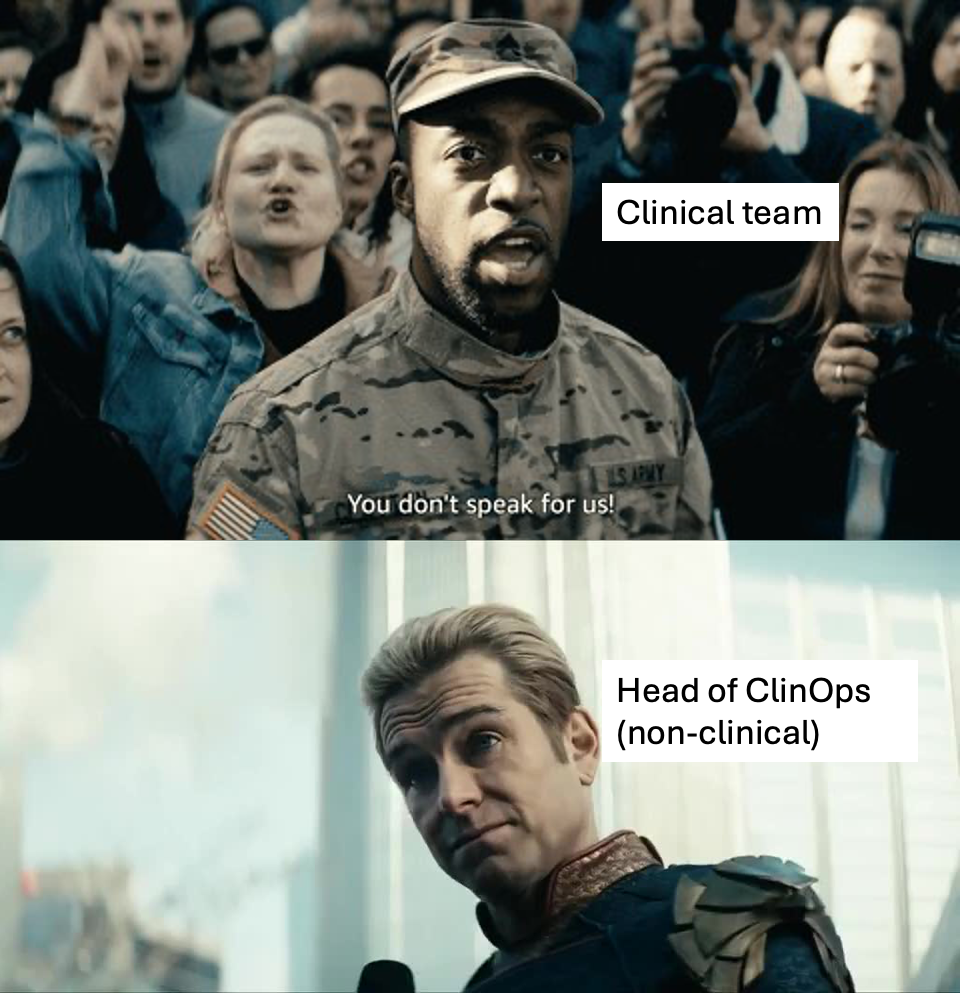
Clinicians need a clinical leader
“If you’re hiring clinicians, you absolutely need a clinician leader to directly manage them. If that clinician leader is an MD or DO, that’s ideal. Otherwise, a smart NP or PA will do the trick. But clinicians speak a certain language, and even if other staff members can speak that jargon and understand their clinical algorithms, there is a certain amount of inherent trust that clinicians share amongst each other (e.g., they both have licenses to lose, maybe they’ve all taken a hippocratic oath, or they’ve had curriculums from endless ethics courses drilled into their brains).
Administrators, no matter how benevolent or selfless they appear, will always be looked with a slightly skeptical POV because there is often a financial incentive for them somewhere. We dealt with this at Bespoke by appointing a Chief Medical Officer who set policies, followed by a Director of Medical Operations who directly managed the rest of our clinicians on a day-to-day basis. If something needed to shift somewhere, there would be an executive discussion, and then the senior clinical leaders would have their marching orders to relay those messages to the rest of the clinical team.”
[NK note: Clinicians just speak a different language to each other. And that language is being desensitized to trauma.
I get the skepticism. It’s the clinician that gets put in a tough situation when tradeoffs are made about business performance and clinical quality. I do think more people that are on the “business” side of healthcare should have to sit in on some visits and hear the patient questions, especially related to efficiency that might impact their quality of care. I get why it doesn’t happen, but a ClinOps person should have to look a patient in the eye when telling them why the visit has to be short, or the doctor can't see them.]
–
There are more clinician hybrids than ever before
“I think one really cool thing from the talent perspective is that a lot of people are going into med school with non-traditional backgrounds, some who know they don't want fully clinical careers. This means you have a lot more people now with a tech, engineering, consulting or finance background who end up going to medical school.
This means the pool of what a clinician can do for your company is much broader than serving as a figurehead. For companies who want meaningful participation from the MD they bring on, they've never had more options to choose from in terms of the additional skill set the clinician can bring whether it's ops, strategy, informatics, product etc. I don't think people are yet realizing this which also may make them more hesitant to spend on this role, but it's something companies should consider.”
-Arjun Gokhale
[NK note: If you can get a software engineer x doctor combo, you’re really hitting the jackpot.
Anecdotal - when I talk to docs that have a combo skillset like this, many of them feel lost because they don’t feel like they’re the best in either field. There’s a lot of imposter syndrome here. If this is you, try to develop a narrative both internally and externally about how few people there are that can crosswalk between having clinical knowledge and X other skillset you have and why that’s important.
For example people that can do large scale data analyses but also have a clinical bend are way better at having a “smell test” to know when some analysis is probably wrong because it doesn’t line up with how patients show up clinically, or how things actually happen in practice. You need to be able to explain your version of that.]
Clinical Co-Founder Dating
“Plenty of rational arguments exist about lack of direct ROI or (potential) drag on startup velocity that comes with clinician involvement. But for healthcare products that impact patients or clinicians, we need to think about things that aren't on the P&L. Who deals with ripple effects of collateral damage when a startup "winds down"? Clinicians often think about time horizons beyond term sheets, and I think better products will get built when those perspectives are in the mix.
We need to have a healthier "dating" environment for founders and clinicians because it's still quite primitive out there. Both sides would benefit from more humility, patience, and effort to align on big picture goals. I'm trying to suggest a different way of thinking (not necessarily a more profitable way) rather than clarifying the reality. The needed culture change is hard to capture in traditional frameworks and that's why I encourage my clinical colleagues to play offense in shaping health tech.
J. Cole actually wrote a song about this whole situation”
-Paulius Miu

[NK note: Wait wasn’t that song about…oh yeah. Quite the edit.
One of my goals for our hackathons specifically is to essentially create a more organic way for tech people and clinicians to get into a room, build cool stuff together, and loosely cofounder date. We are trying to bring this concept to hospitals, so if you’re at a hospital and want to make this happen let me know.
I think everyone could learn more from each other.]
—
Oh, the clinician archetypes you’ll see!
I’ve seen quality range a lot from (not mutually exclusive nor comprehensive):
1) “I am a doctor treat me like a loyalty” type hands off advisors
2) “hands on but heads down” type - contribute to operations but too aloof with “health tech” market
3) “what’s a cap table” type but super helpful and clinicians who have no idea what startups really want to do - grow and exit
4) the ever-on superhuman clinician-entrepreneur-family men and women who humble you.
YMMV - I have trouble pinning down what should be the archetype of clinician that work well in a “healthcare startup”. Avoid #1 for sure but you can’t have a clinician who doesn’t understand the world outside of the startup or medicine (2 or 3). #4 is rare and just might be a byproduct of timing (having entered and exited during golden era of digital health).
Long winded way to say “I don’t know” but I think compensation expectation needs to be toned down specifically for physicians.
One thing to note - no one will pay you clinical practice salary (unless you are doing clinical work for the startup) - keep it in tune with what would make the startup successful while being fairly compensated.
Personally, I’d err on the side of two founding engineers if I were a digital health company - gives you the agility to build fast, fail fast and pivot as needed. And clinicians often would deviate to the workflow of clinical medicine, which may just result in slow burn rather than fail fast.
[NK note: Wait till you hear about much the founding engineers want, you might change your tone. Also lets be honest, no employee understands the cap table.]
—
There are good and bad people regardless of degree
“Somewhat related, there is one thing in this discourse that I find super annoying and it also bleeds into the “private equity ruins healthcare” discussion that is so prevalent (and spoiler alert: yes private equity has ruined some healthcare companies). I come across many people who believe that having a clinician on your leadership team automatically means your company cares about patient care and if your leadership team is made up of MBA’s, the company only cares about making money.
I particularly notice it in the behavioral health and hospital industries. It’s such a gross generalization that presumes both that someone with an MBA is incapable of making decisions that put patient well-being over profit AND that physicians leading businesses don’t care about money at all. In reality there is so much more nuance to this. I know MBA non-clinician founders who are incredibly compassionate people who would never compromise on patient care in a million years and I know physicians that would do almost anything (even illegal stuff) if it meant bringing more money to their practice/company. And plenty of examples of the opposite situations as well.
My point here when it comes to having clinicians on a leadership team, I think the decision should be made based on the operational expertise needed and how a clinician directly serves the business. What I think is wrong is judging the motives of the leadership team members of a startup based entirely on the letters following their names. That shit needs to go."
-Anonymous
[NK note: Wait so what am I supposed to think about a PE firm that is run by a doc? That’s a combo that will make algobrained readers short circuit.
While I do broadly agree with this sentiment, the one nitpick I will say is that clinicians in leadership take on more personal consequences when things go wrong in a clinical model vs. someone running a private equity firm that typically has many layers of shielding. You do something gray as a doctor, that travels with you on your medical license in a way so you have more to lose.
But sentiment wise I agree - it comes down to an individual’s character and motivation which is totally independent of their degree]
Practice? We talking about practice?
“As an MD that briefly considered quitting residency during covid to go into industry, I'm glad I finished training. The clinical understanding of truly practicing medicine in residency and then independently can only be gained through experience. Finishing my clinical training and now practicing as an attending, has led me to conclude that what I learned in medical school was a fraction, maybe 20%, of my total medical/clinical expertise.
Having now become a practicing physician, the “MD/MBA I realized I didn’t want to go into residency” you alluded to, really has a fancy biology degree with a modicum of clinical context. I know this is also a sentiment shared by my medical school friends who are also innovation inclined and completed clinical training. I think a clinically-trained vs a non-clinically-trained MD/DO will likely have significantly different expertise to contribute in industry, although I'm sure there is some amount of overlap"
[NK note: Which part of the degree is more divorced from reality, the MD or the MBA lol. Jk I love you MD/MBA friends, you’re keeping the critical healthcare consulting industry alive.]
Thinkboi out,
Nikhil aka. “I need a doctor ft. Eminem and Skylar Grey”
Twitter: @nikillinit
IG: @outofpockethealth
Other posts: outofpocket.health/posts
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







