How to fight hospitals!!! Some more ideas
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
This episode of Out-Of-Pocket is brought to you by…
Health insurance sucks! It's confusing, expensive, and gets in the way of care. Arlo is an AI-first health plan for small businesses. We put our members front and center, using AI to make their healthcare journey simple and clear.
In just over a year, we're active in 30+ states, serving hundreds of businesses. We're expanding our team across sales, engineering, and other functions. Want to join a high-growth company and help us fix this?
--> Join Us!
Manifesting hospital competition
Last time I wrote a manifesto about how we should increase competition in the hospital sector. I got SO MANY thoughtful emails about ideas people have been thinking about, clearly I struck a chord.
Below are my favorite ones - which include firsthand stories from physicians getting boxed out, some interesting ways to get the military involved, and different fee structures to look at. I think the fact that most people asked to be anonymous already says a lot.
Memes and notes at the end by Nikhil, commentary by contributors
The Non-Competes That Stop Bundles
“More important than the CON laws blocking competition and lowering prices are the non-compete clauses in physician’s employment contracts with hospitals and PE firms and ASC ownership contracts that prevent physicians from contracting directly with employers to lower prices.
USPI/Tenet is the managing partner in about 500 ASCs nationwide. They are currently blocking over 15 orthopedic groups with 48 ASCs nationwide from offering transparent surgical bundle prices for ASC orthopedic surgeries on marketplaces like Tendo. These marketplace rates are usually 5-10K cheaper for an orthopedic surgery than using commercial insurance at a hospital because the surgeon can shop around the facility fee to different ASCs. These orthopedic groups need USPI to agree to a facility fee, but USPI refuse to give any negotiating power to physicians because physicians control the top of USPI’s funnel. Over time, physicians would shop the facility fee around, and USPI does not want that pricing pressure.
Every ASC in Nashville is controlled by a hospital who block surgeon controlled surgical bundles on these direct to employer marketplaces. My group, TOA, has been in contract negotiations with USPI who manages our surgery centers for >2 years and their answer is typically, “the contract is with our lawyers and we will let you know something next month.”
Healthcare is like the saran ball wrap challenge where you keep trying to get to the core but just keep finding one more obstacle after another.”
- Anonymous

[NK note: It’s worth describing the dynamic here. When you need surgery, your surgeon will typically pick the surgery center. Therefore surgeons control the top of the funnel for those centers.
Today, most independent surgeons are locked into operating at specific Ambulatory Surgery Centers through their ownership or partnership contracts (they’re typically 49% or lower ownership). My understanding is that this is partially because the Certificate of Need laws basically favor getting hospital buy-in to get the facilities approved.
The surgeons don’t really have visibility into what the facility charges separately. Frankly most probably don’t really care because the payer will pay the surgeon and the facility separately.
But let’s say a surgeon wants to list a transparent all-in bundle that INCLUDES the facility fee. Maybe they want to go directly to employers and offer this. Then the surgeon would have to care about that facility fee since it comes from their bundle. But that also means that the surgeon would shop around different centers to get that fee down. The surgeon would also likely make more from that bundle vs. what they get from whatever their partnership is with the surgery center.
Honestly I always thought surgeons had all the leverage in any of these transactions, but maybe my viewpoint needs to be re-evaluated.]
Quick interlude - Healthcare 101 + Hackathon Sponsorship
Just a reminder…the healthcare 101 course is officially enrolling!!! Starting 3/23, I’ll teach you everything you need to know about how healthcare works.
I know it seems like I’m just always joking, but keeping things entertaining is a critical part of keeping people engaged and learning. If you care about your people actually learning the material and not just checking the box, you should sign them up.
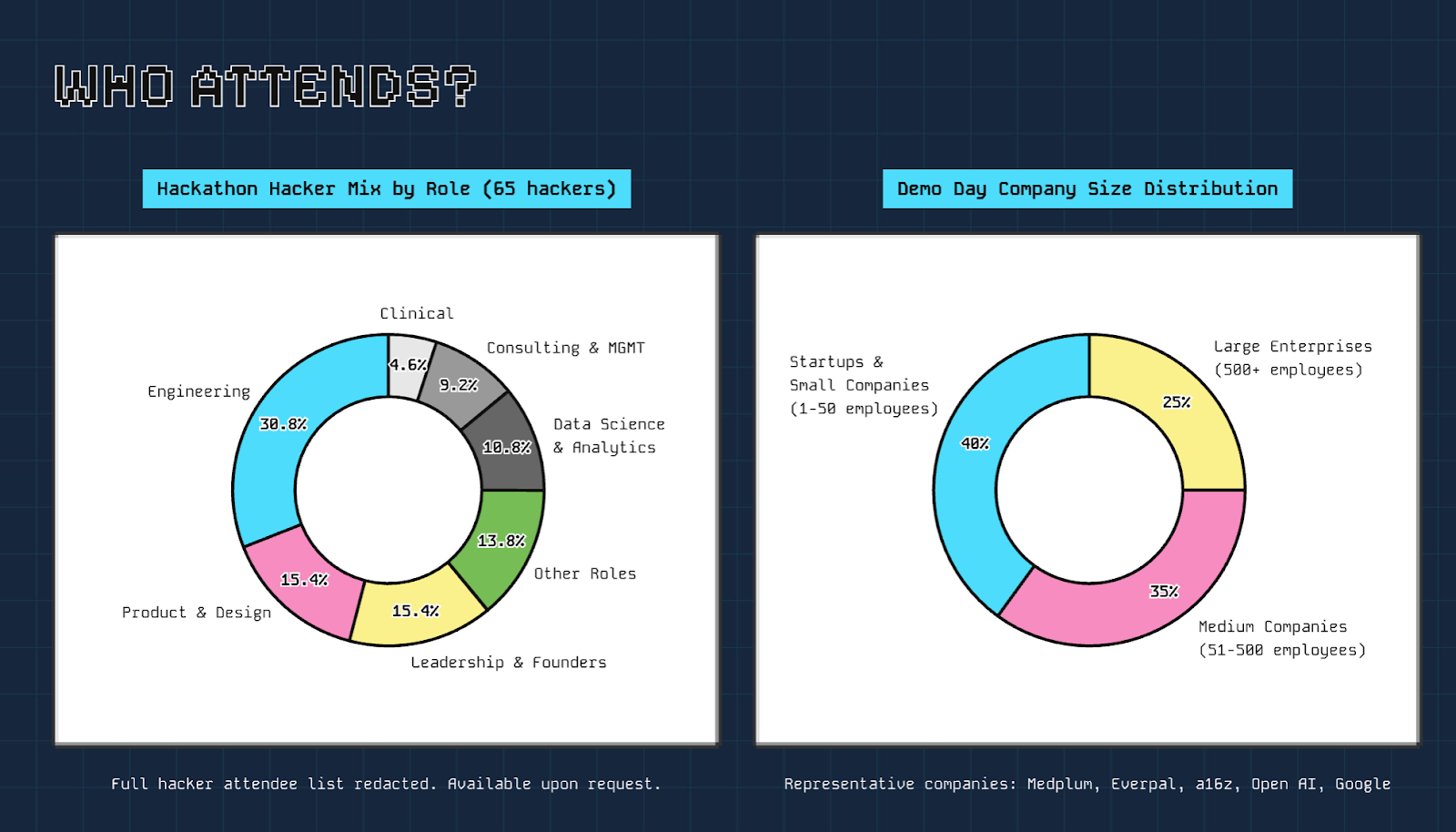
Separately, we got more than 230 applicants for our healthcare hardware hackathon in April!!! Probably one of the most impressive batches so far - we got people from Nvidia, Boston Surgical, Apple, Kaiser, and more that are excited to build.
We also have locked in our first sponsors, which I'm excited to announce soon 👀 We have a handful more sponsorship slots so if you're interested let us know sooner than later.
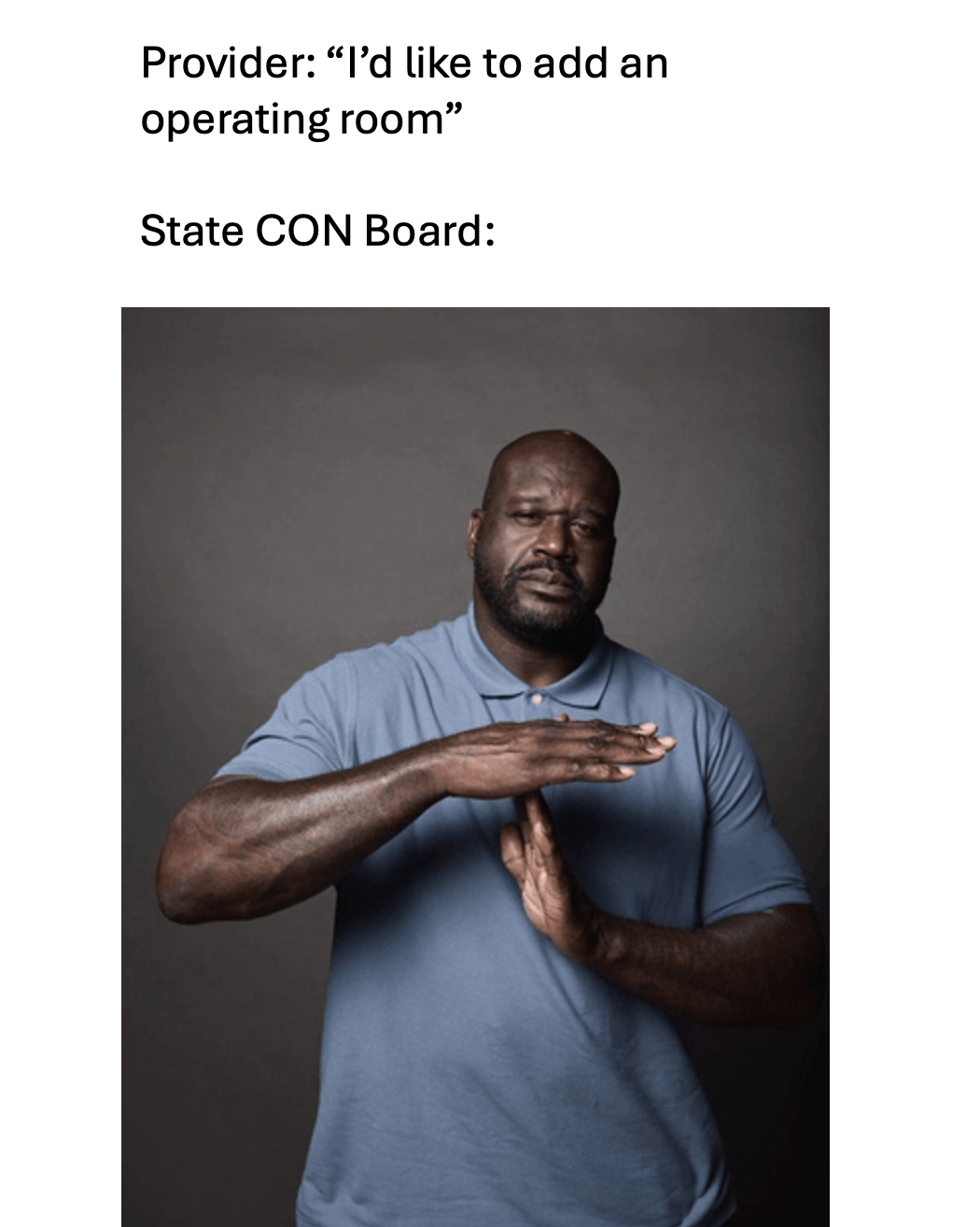
The History of Certificate of Need
“Historical context plays a huge role in this conversation. The 70-80s were an era of supply driven demand where doctors ran amok owning and exploitatively profiting off their medical services. This is why CON exists and why doctors can’t own hospitals. Given this new era of price transparency and attempted competition, CON has largely outlived its purpose. As far as doctors ownership, I think if that was allowed they would abuse it again (saying that as a doc). I’m for loosening ownership rules but not getting rid of them.
Doctors got punished for abusing their power and site neutral payments should be the natural punishment for hospitals abusing facility fees. There is logic behind why they exist but it’s been exploited and needs to go.
Noncompetes in healthcare are dumb. If the hospital or practice actually provided anything proprietary, they wouldn’t try so hard to imprison their doctors by contract. Physicians aren’t taking workflows or IP with them when they leave, just their skills which is what the people want and doesn’t come from the system.“
[NK note: In general I think healthcare has lots of rules that were designed to prevent bad behavior during a time where it was way harder to audit people and enforce rules. Guess that’s why they call it the CON law.
My general belief is that 70-80% of egregious bad behavior is usually done by <10% of physicians, don’t quote me on this just a vibe. If we monitored and enforced actions against particular suspicious docs abusing things like self-referrals and consistently recommending unnecessary care, I feel like we could catch that way more easily now.
Though I say that and then there’s headlines like “$8B of Medicare fraud committed over the last 5 years” so maybe not.]
–
340B pricing is the hospital’s edge
One major driver of hospital consolidation that rarely gets discussed is the 340B Drug Pricing Program. Under 340B, hospitals can purchase outpatient drugs at steep discounts, often around 50%, and keep the full spread when insurers reimburse at list price. That spread is enormous, exceeding $70 billion annually. Critically, this subsidy is unavailable to independent physician practices. As an example, if an independent oncologist administers chemotherapy, they pay full price for the drug. If a hospital system buys that practice, the discount suddenly applies, increasing net revenue. This creates a powerful, policy-engineered incentive for hospitals to acquire community practices. Many research studies, including GAO and Senate HELP Committee reports show that hospitals frequently use 340B profits to fuel consolidation and expand into wealthier, commercially insured areas, undercutting the program’s stated safety-net purpose while driving prices higher system-wide.
Administrative burden and Stark Law compound the problem by structurally favoring large systems over independent physicians. CPT requirements are bad enough, but modern Medicare also includes layers of quality reporting, compliance, and documentation that require large, permanent administrative staffs. Hospitals can absorb these fixed costs through scale, unable to be matched by independent practices. Stark Law further tilts the field by imposing complex self-referral restrictions exclusively on physicians. An independent doctor who wants to own imaging equipment must navigate a compliance minefield, while hospitals can freely own, operate, and self-refer with minimal friction. This makes it difficult for independent practices to scale while hospitals can do so while issuing tax-free bonds.
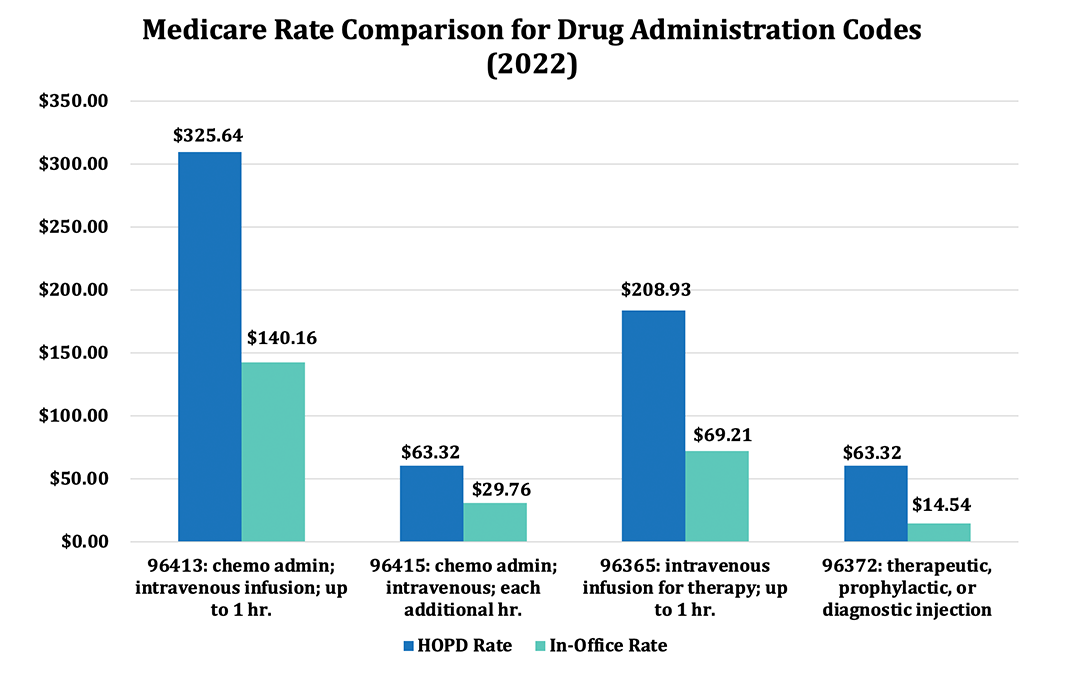
[NK Note: The 340B program - we’ve talked about many times in the past. It does seem like as more of the fights happen around infused drugs in particular (where you can play quite a bit of billing shenanigans and the CPT codes have very high delta between hospital and independent clinics).
Stark Law feels a bit like the Bible - everyone seems to have a different interpretation and risk tolerance for what counts as bad. I’ve seen lots of pretty creative structures to effectively get around Stark Law, but that again works against small practices. 1 Peter 5:7 in the Stark Bible.]
–
Military Hospital Takeover
“For sure the best way to increase hospital competition is to eliminate Medicare (~$1.4T/yr), redirect that spend into a dramatic increase in military funding.
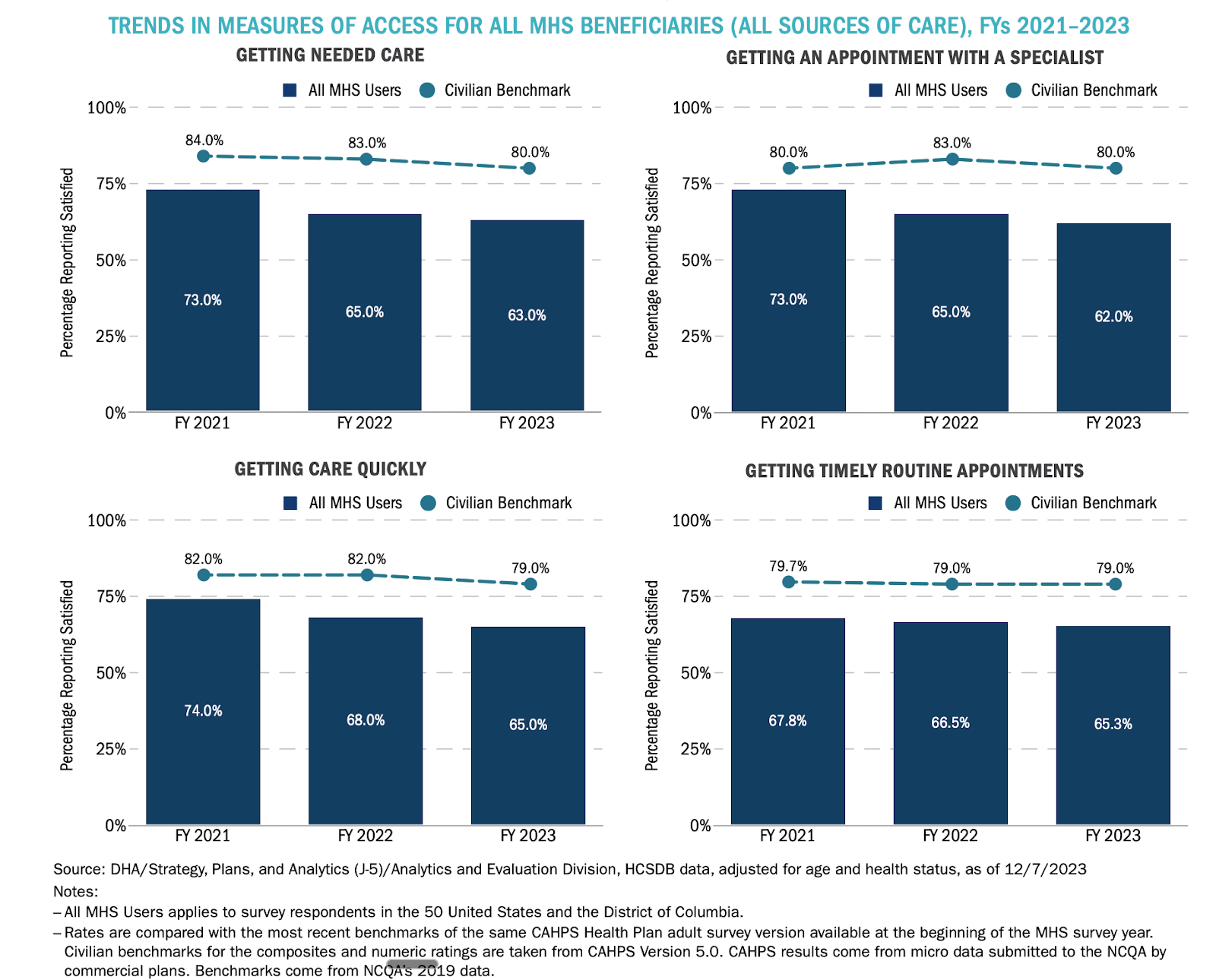
Rapidly scale military run hospitals and clinics that are open to Medicare- and Medicaid-eligible Americans (or why not all Americans while we’re at it). Take over failing rural hospitals and underused infrastructure (including empty malls), massively expand training pipelines for generalists and military clinicians, and allow the federal system to deliver core hospital services at scale. The result would be a large, price-disciplined competitor in nearly every market—one that forces private hospitals to compete on cost and quality rather than leverage and consolidation—while being politically legible as a national security and readiness investment rather than another incremental healthcare reform. US military spends about $5.5k per covered life, so could cover all 330M Americans for about $1.9T… we’re not so far off :)
This feels like an appropriations bill both parties could get behind - “massively increase military funding” (just don’t mention the S-word).
Inspired by Aug 2019 Health Affairs -
https://www.healthaffairs.org/toc/hlthaff/38/8”
- Alden Mitchell
[NK note: I did ask for out there ideas and this one checks that box. I feel like the VA and TRICARE is…fine? It’s an interesting idea to provide VA level of service to everyone that wants it, and then the other hospitals basically have to compete against that. Many other countries do that and I think it’s probably a good idea. Just tell them the old hospitals have oil in them and get this party started.]
From a doc in Texas - the plight of cost-based reimbursement
“I'm a urologic surgeon in Texas. I have many, many thoughts on this...
I would take the reimbursement framing even further - reward procedures outside of a hospital. Hospitals are incentivized to bring in as many procedures as they can, even if these are simple and "low reimbursement" because of the reimbursement spread created by facility fees. Let me enlighten you into the ridiculousness of the incentive scheme in my world. As I tell the medical students and residents, perverse incentives drive bad behavior.
I'm in a fairly large single specialty group. We do a lot of prostate biopsies to check for prostate cancer. I mean like >1000/yr. Average reimbursement in 2025 for this was about $367. Not too bad right? Ehh, not so fast. Procedure takes 30 min, is labor intensive for staff, cost of biopsy needle ~$70, reprocessing equipment, sedation, depreciation of a $50k ultrasound machine, overhead, etc. So rough net profit is ~$100 But wait. Don't we want to be able to target any suspicious areas of the prostate instead of just shotgunning this thing? (side note, up until a few years ago that's exactly what urologists did - random sampling with a crappy ultrasound image :/). Why yes, that would be a good idea to target any suspicious areas in the thing you're concerned may have cancer. Good thing there are MRI's to help us find them and good thing there is hardware/software we can use to make sure we can accurately sample these spots in real time.
Wait - CMS, you say you're only going to pay for the ultrasound biopsy part because the outdated CPT is so generic it doesn't even consider the MRI fusion hardware? This equipment costs around $300k dollars to purchase, not to mention paying a radiologist to read/map each image. So groups just rent it, usually adding around $500 extra cost per patient. So that $100 net is now a negative $400.
[Side note. Yes, we've run all the possible scenarios on purchase of equipment and every scenario is still a financial loss on each biopsy. We also get preferred rental pricing because of the size of our group.]
So how do we reconcile this? No one is gonna perform procedures that net their clinic a negative $400 and you can't just stop doing biopsies. So up until a month ago, groups like mine would charge an ABN (Advanced Beneficiary Notice essentially telling the patient that their insurance will cover the ultrasound biopsy portion but won't cover the cost of the MRI fusion equipment and the patient will be personally billed for that specific, uncovered service). So patient pays more for the biopsy but it's still a viable office based procedure and the patients are still provided a necessary service and it's much cheaper for the patient than doing at the hospital.
2026 rolls around and new CPT codes for prostate biopsy are here. Great right? Codes are now accurate to current procedure by including the MRI fusion part. Reimbursement is up to a whopping $417.66 from $367 due to the "increased equipment cost". However, because the CPT code accurately includes the MRI fusion portion we are no longer able to have patients sign an ABN. What does this mean? It means that groups who rent this equipment are now required to foot the entire cost of the procedure, meaning it is now a $350 loss for each and every biopsy. This is a no-go. What does one do? The only thing one can... shift the costs somewhere else - a hospital or ASC.
What happens next? We call the Hospital/ASC saying we need to do biopsies and they contract with the rental company to provide the equipment and biopsies are now done in the OR. How does this play out? Well CMS now provides $1700 to an ASC and $3600 to a hospital to provide these services. And don't forget that hospitals received a 2.6% increase in outpatient OPPS rates in 2026 :). For the hospital in particular this is now a lucrative, highly efficient and high-throughput procedure. For the physician, it's a poor use of OR block time and is reimbursed ~$150 when done in a facility. For the patient, they are now having an actual surgery with all the financial trimmings - facility fees, anesthesia, etc., including a much higher cost on average.
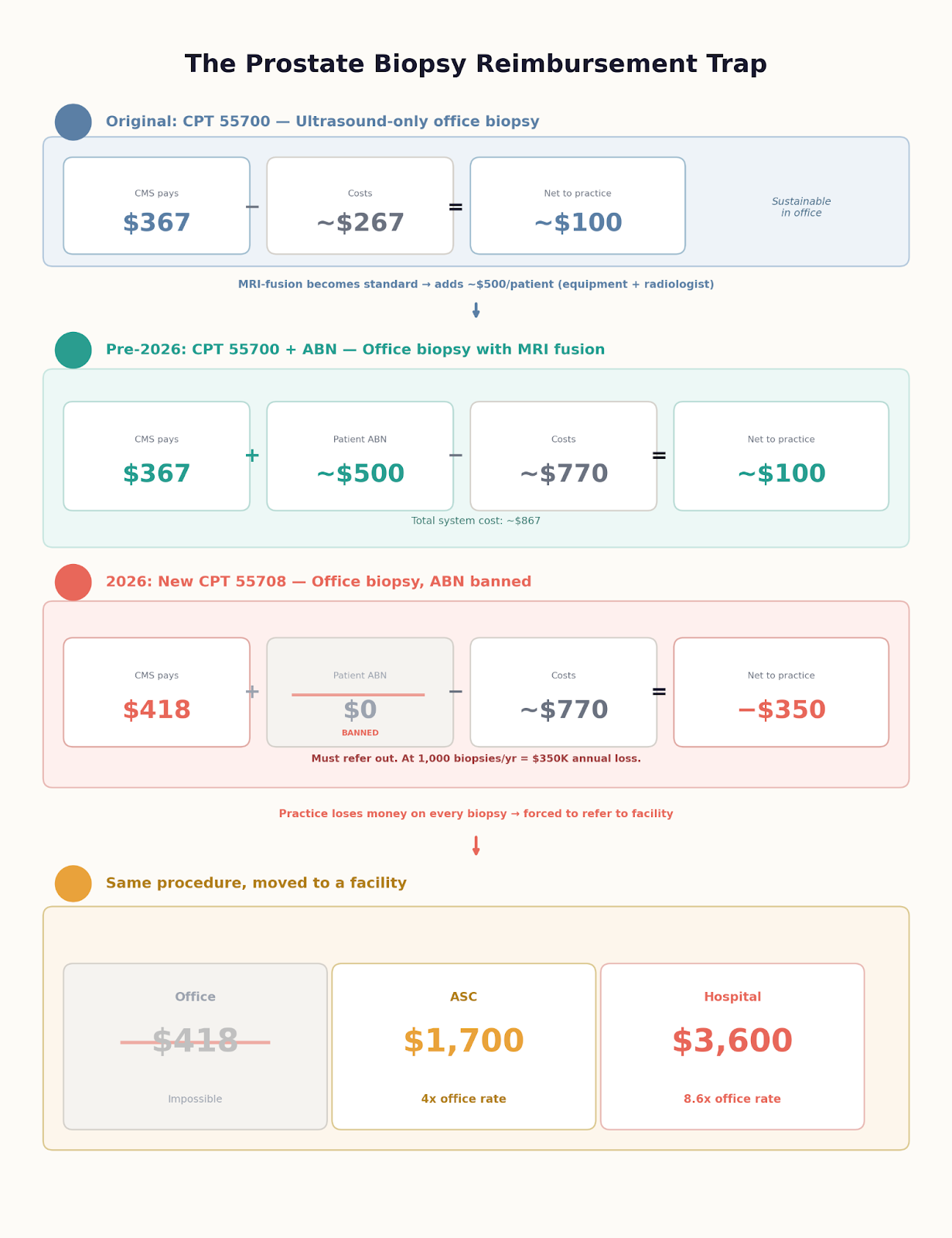
Why does CMS think it "costs" over twice as much to perform this at a hospital compared to an ASC? It's definitely not because the turnover time between cases is quicker! It's definitely not because they require more staff to perform the same procedure. It's because the subsidization of hospital care is slushy and spills over into all these other procedures. Steel manning this, we're trying to make hospitals whole due to some of the uncompensated care they provide but we're doing it by disregarding the fact that it costs the entire system an order of magnitude more money to do the same procedure at a facility compared to a clinic setting. In this example, we're forcing physicians (and patients) to utilize far more resources to do the same thing.
What do you think the hospital said when I asked them if we could start performing biopsies in the OR? I may or may not have gotten a text from the CFO asking what he can personally do to help make this happen.
Anyways, I guess my point (which may not be clear due to all the ranting) is that, while healthcare costs are extremely complex and many look at hospitals as community care monopolies, there are some fairly visible (to those inside) inefficiencies that have strengthened that monopoly in unusual ways. Does keeping "routine" procedures out of hospitals help increase hospital competition? It absolutely does IF one defines a hospital as an institution that receives it's revenue from high acuity care instead of one that uses low acuity outpatient services to subsidize high acuity care (and put a nice Steinway in the atrium). The latter is currently how CMS defines it and it proves this because of it's payment incentives.
Pee-PeeDocboi out”
- Anonymous
[NK note: I cannot believe I got a urologist to sign off as Pee-PeeDocboi. This is literally the highest accolade I’ve ever received.
This was a crazy read. Two specific standouts:
1) I learned about what Advanced Beneficiary Notices are, and when I asked if patients actually paid them the doc said they grumbled a bit but were fine with it. This is a rabbithole I gotta go farther down, and I’m curious if any of you use them regularly.
2) This feels like one of the core flaws of CMS and the CPT coding system that uses “how much did that cost” as the baseline for figuring out reimbursement. Of course if you use that methodology you will end up with people shifting care to higher cost settings.
Some thoughts about site of care
“Move away from “site neutral” payment – a race to the bottom – and focus on “site of care optimization.”
- “Site neutrality” just hurts hospitals rather than boosts reimbursement for independent docs/ASCs, so politically it’s not all that helpful (and who wants to take on the hospital lobby).
- Plus, there are a lot of political reasons why it’s really hard to do (for example: ASCs aren’t required to submit cost reports, so coming up with a “fair” price is actually impossible right now, because we don’t know how much it costs to do things in ASCs”
- Instead, can we focus on market-driven mechanisms for shifting volume in a way that naturally reduces costs (like a lot of what you described) versus just slashing payments (which is politically impossible for surgeries in particular)
What can you actually do to optimize site of care?
- So glad you asked! There have been policies in place to shift care to lower-cost settings, namely the Inpatient Only List (IPO) and the ASC covered procedures list (CPL).
- CMS just significantly expanded this list this year and is trying to get rid of the IPO for the second time (Trump 1 did it and Biden put it back in place after an outcry about safety yadda yadda). They’ve changed ASC CPL criteria to be more about clinical decision-making than a super specific set of clinical criteria.
- BUT – the question remains – is there a natural plateau that happens in the amount of care that shifts, primarily due to the structural things you outline below (CON laws, consolidation, noncompetes?)
If the answer to this is yes , then what can you do to incentivize docs to shift more of the care?
- Private payers are doing this in a few ways:
- through $0 copays for patients to get things done in ASCs vs HOPDs – it’s working!
- They’re also paying higher professional fees for ASC cases vs. HOPD cases – as seen in the paper I linked above, even the data shows that pro fees might be higher in the ASC, but net net these payers are still saving 25%+ on these cases
- But what about Medicare?
- Right now, in the MPFS, Medicare pays a “non-facility” or a “facility” professional fee. In the 2026 rule, they slashed the facility-based rates significantly, citing hospital consolidation – specifically, their rationale was – “if you are a doc who joined a hospital, you don’t have your own office to maintain anymore, so you shouldn’t have that built into your practice expense RVUs, so we’re cutting those by 50%”
- This is a great argument, except for the fact that it has the same impact for HOPD and ASC-based surgeries (SNF-based care also got tied up in this, which was seemingly an unintended consequence but CMS DGAF). The only distinction in the MPFS is “facility or not a facility” – the facility distinction comes in the facility fee, which is governed by the OPPS.
- My idea: how do we update the fee schedule so that there is a [Site of Care]-specific professional fee that accounts for the differences in care at a hospital and an ASC? Would this increase the pro fees for ASC-based care? (probably/hopefully)
- There are many practical reasons why you can’t do this today – not the least of which is that the MPFS is by definition budget neutral, so Congress would have to step in and authorize this type of change – but it’s not crazy!”
-Anonymous
[NK note: The acronyms are making me wonder if I’m having a stroke, and whether I should go to a HOPD or ASC to get it fixed.
General gist here is we should create different fees that incentivize more procedures in ambulatory surgery centers (ASC). You can do this by waiving co-pays which employers are doing, or you could instead boost the surgeon’s fee for doing it at the ASC. The main question is how much leverage the surgeon has in choosing where it gets done.]
The Non-Profit Hospital Power
“some other things to consider related to non-profits specifically:
- Hospitals have huge fixed costs and once they commit to new towers, etc, they have to fund the debt/bonds, etc. And rarely does anyone actually want their local hospital to go under so once the money is spent on a new bed tower or OR's or whatever, then that's just gonna be thrown in the balance sheet and income statement of what's needed in the rates to stay afloat. There's probably not enough scrutiny on the decision of hospitals to add more beds / build new tower etc since rates will inevitably have to adjust to keep up with costs
- The boards of most major hospitals are the most powerful / wealthiest people in the community. They have vested interest in hospital making money / staying profitable and if there is legislation or rate changes, etc that might impact that, you better believe that politician (who also prob gets campaign checks from those same folks) will hear about it. Very difficult to bring meaningful new policy due to these dynamics
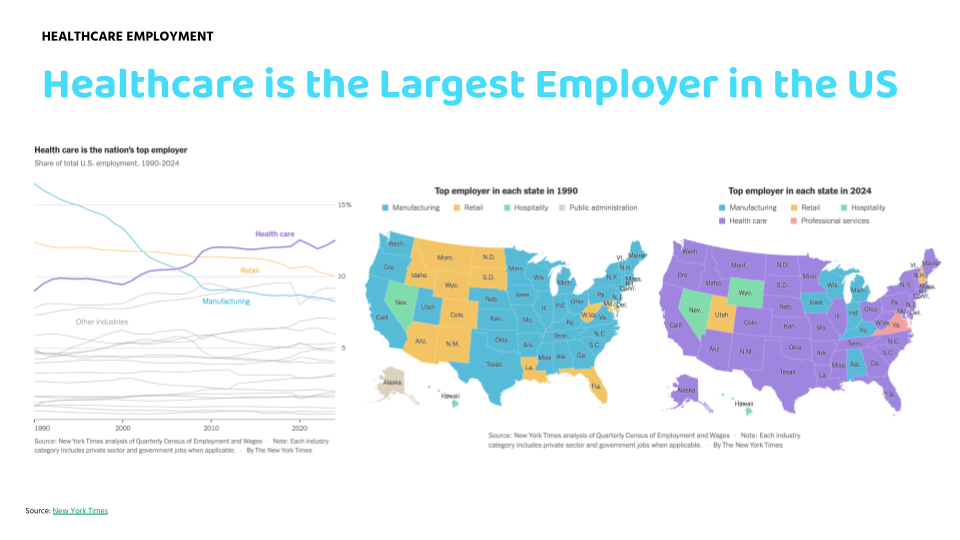
- Similarly, hospitals are typically the largest employers in the town/community/city and eliminating roles dampens local economic activity
- Of course, one of the counters to all this is that when you get sick or I get sick, I want the best hospital, nicest place, lowest nurse:patient staffing ratio, etc, so there's also real tension in what we want when seeing premiums increase BUT when we actually need the service and you have to be admitted to hospital (which inevitably means it is somewhat serious) spare no expense, just get me better (which is completely normal).
Beyond changing laws/regulations, the best antidote is the large local employers who foot the employer sponsored insurance bills at least asking questions / scrutinizing the terms. None of us really believe the benefits brokers or HR depts in most companies understand (or have access to) claims data to ask the right questions and serve as a counterbalance to hospital control. Like or hate Mark Cuban, I applaud his public pus to CEO's to pay more attention to their healthcare costs and scrutinize the data / push their brokers / ensure TPA isn't paid off total costs etc
- Anon physician leader that used to work at a large non-profit health system
[NK Note: The intertwining of healthcare jobs and local politics is one of the first things we talk about in the healthcare 101 course. It’s not just jobs, but your local social stature as well - being on the board of the largest health system in your area makes you seem powerful.
–
The German perspective
In Germany right now there’s an active push toward *reducing* the number of hospitals and consolidating services. A big reason is quality and operational viability: for complex procedures, outcomes tend to be better when teams perform them frequently (and it’s hard to keep specialized staff, nursing coverage, etc. sustainable at many small sites). Because prices are much more regulated here, the consolidation debate isn’t primarily about “market power and negotiated rates,” but more about outcomes, staffing, and whether the system can run efficiently overall. And since the system is collectively financed (ultimately by workers and the state), there’s also a strong focus on total cost of care at the system level (not perfectly, but much more than in the US I suppose). So if you duplicate expensive infrastructure everywhere, everyone pays for it one way or another.
Reading your argument made me wonder if part of the answer in the U.S. is to reframe “more competition” as something that should be targeted: increase competition for routine, “shoppable” care while still actively protecting quality for complex care through centralization and
standards. For example, for complex procedures you could have minimum-volume requirements before a hospital can offer them (something that is currently being discussed in Germany), plus outcome transparency (registries/reporting) so performance is visible. That’s been discussed here as well, the idea being that if a site performs poorly on a given procedure, patients (and referring physicians) can respond.
Then on the routine side, your points on site-neutral payments really resonated as a major lever. Even from the outside, it seems like paying more for the same service just because of hospital ownership creates exactly the incentives you described (acquiring clinics, shifting billing codes, etc.) and makes it harder for independent entrants to compete. I don’t have substantially better ideas than the ones you already laid out, but the main thing I’d emphasize is the segmentation: “competition where it makes sense, concentration where it improves outcomes.”
Curious how you think about that framing: centralize complex care deliberately (with standards + outcomes transparency), but push harder on competition/payment neutrality for routine care so price pressure shows up where patients can actually choose.
- Clara Schoenwald
[NK note: I actually had this conversation with someone after the piece last week around trauma centers - you actually want all the traumas in an area to go through one center so people get practice and get better. Spreading them out also spreads the expertise, and since patients don’t shop for trauma centers it makes each individual center worse off.
I can see the argument for having fewer of these. But you need to figure out the price setting mechanism for entities that benefit from essentially being monopolies. It seems like Germany does through government intervention.
The tradeoff though is that the US is the best in the world for complex care because of totally uncapped dollars. Always interesting to hear how other countries deal with it]
New training models
A common theme in the challenges you raised is that doctors spreading their medical wealth is key to driving competition, but they have a lot less agency than they'd need to make a change. So I think a change in competition has to start at the bottom - when doctors are first coming out of school how do you get them to consider not selling their soul to those top hospitals and getting locked into the gold non-compete handcuffs?
Thailand (and maybe some other countries, but I'm not that educated) actually has a pretty interesting medical training model that could cause a stir:
The majority of students have a government subsidy for med school, which means much less debt coming out, so less need to fight for the shiniest job to survive. As an added bonus (for this narrative at least, maybe not for them), the "catch" to the government subsidy is that those students have to work in a public hospital for 3 years before they can mosey on over to a cushy private gig. Not all students get that subsidy, but (without any data except all the movies I've seen that tell me the rich kids are cool and don't try hard at anything) I doubt the 20% that paid for school themselves are the top 20% of every class.
That means that for at least 3 years the medical talent from each class is spread out more evenly. Private hospitals might still be better overall, but the gap closed a little bit. Now let's say you stick a magical money genie (celebrity, non-hospital company, government program...) in this situation and now after 3 years you have some top students with little debt, no non-competes, and a magical genie luring them into going to the new hipster neighborhood hospital instead of their ivy competitor downtown.
Breaking the talent monopoly could be a foundational crack in the dominant players self-reinforcing superiority.
-Andrew Bohannon
[NK note: This idea is really interesting. In the US we have some programs like this for loan forgiveness if you work in shortage areas, but I like the idea of blanket doing it for all docs. If you look at schools where tuition is now free (e.g. NYU), it turns out having less debt didn't really change much and people went to high paying specialties because they like money lol.
But, I do think that it’s not fair if docs are the only ones that have to do this - they already have enough delayed gratification of income. Honestly maybe we should all do this after any higher education??]
Conclusion and parting thoughts
These were awesome. I really feel so lucky and privileged that people are willing to share this stuff with me. I learn a lot from you guys, and maybe some of these stories will reach regulators to make some changes!
Thinkboi out,
Nikhil aka. “ABN Nahmir” aka. “ASC about me”
Twitter: @nikillinit
IG: @outofpockethealth
Other posts: outofpocket.health/posts
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







