The new wave of Radiology AI companies
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Network Effects: Interoperability 101
.gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
This episode of Out-Of-Pocket is brought to you by…
Health tech is one of the biggest opportunities of our generation, but navigating clinical workflows, AI models, payer portals, RCM, countless EMR systems, and HIPAA requirements can quickly slow innovation. By partnering with a healthcare-experienced development team like MINDK, you can stay focused on what to build — while we take care of the how. We help both large organizations and startups.
Introduction - Radiology AI seems more promising
Many months ago, Ayushi Sinha wrote a guest post on why the first wave of Radiology AI startups didn’t work out based on her experience working at one.
People really enjoyed it, so we teamed up again to do part 2. This one is about how the new wave of radiology companies are trying out different approaches that seem more promising. Memes and commentary by me
My title of “Is AI RAD now?” got killed, I tried.
Why Radiology AI today might be different
By Ayushi Sinha
At Nines, we had FDA-cleared models, promising clinical results, and massive datasets. And yet, Wave 1 didn’t deliver (e.g. hedge-filled reports that broke NLP, brittle models that failed on edge cases, clunky workflows, unclear reimbursement, and business models that didn’t fit the healthcare market).
So why do I think it’s going to work this time?
- The tech stack is more mature, bringing down model development costs.
- The business models are better and capture more value.
- Distribution and workflow are the focus.
- Regulatory guidance for AI/ML medical devices has matured, reducing approval risk and timeline ambiguity.
- And the funding environment is more flexible.
Here’s what’s changed and why I’m hopeful for Wave 2.
Wave 2 is workflow focused
One big shift in the second wave of radiology AI is where companies are starting. While many market themselves as “AI-first,” the initial wedge is deliberately unglamorous: build great workflow infrastructure and add AI later.
In particular, many are focused on reinventing the Picture Archiving and Communication System (PACS), the core imaging software radiologists use daily. PACS…leaves a lot to be desired. The legacy systems are slow, poorly integrated, click-heavy, and deeply frustrating to use. But what if it was good, actually? New AI companies are developing alternatives that use a workflow that radiologists already use (PACS) and instead making it better.
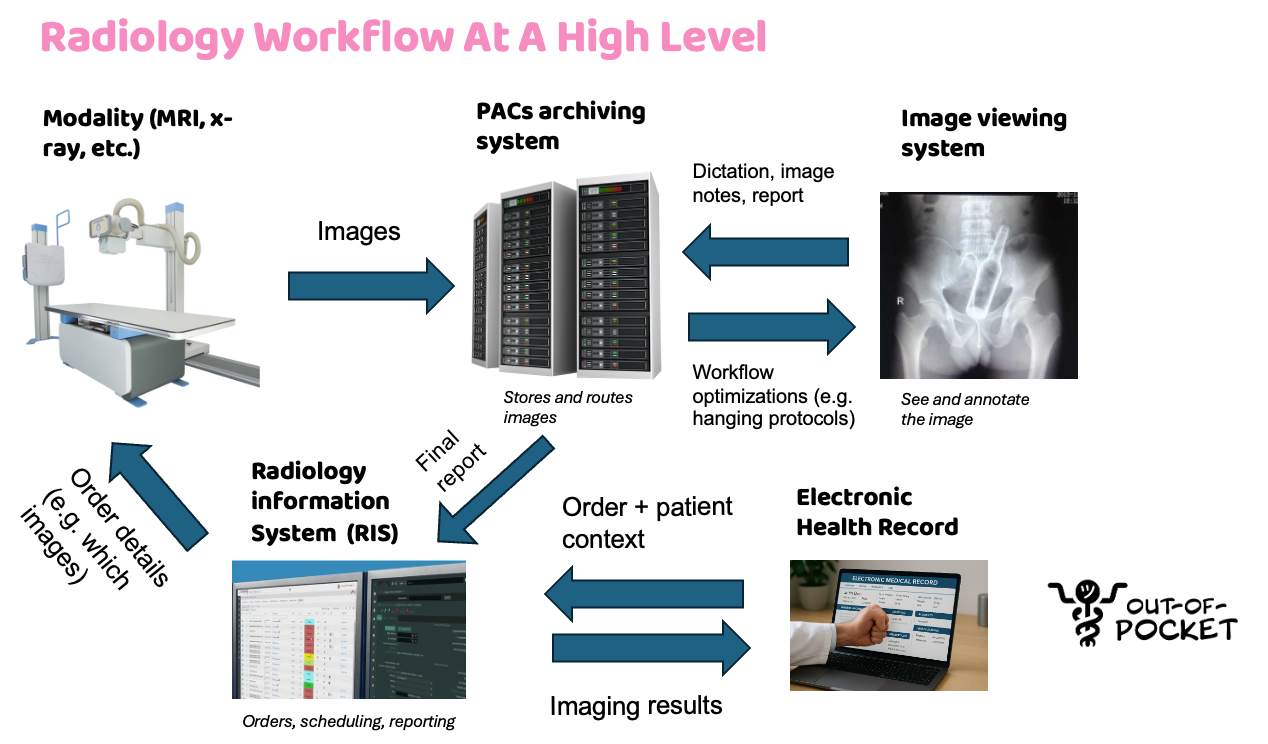
Wave 2 companies are accelerating workflow instead of doing the diagnoses themselves. It doesn’t render clinical judgments or replace the radiologist. Instead, it helps them move faster and make the diagnosis themselves, through better routing, hanging protocols, dictation assists, structured templates, and QA for completeness. Staying non-diagnostic makes it easier to launch quickly and build trust by being collaborative.
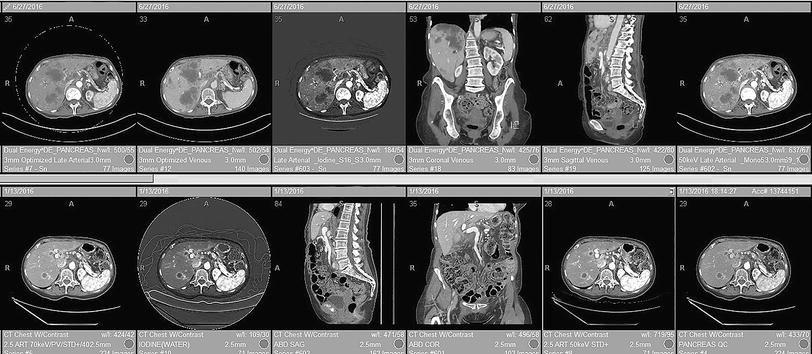
Let’s look at a specific example: hanging protocols. Hanging protocols are the rules a viewer uses to load and arrange images (e.g. what series appears where, which prior image sits side-by-side, and what window/level presets apply for each modality and body part). In practice they’re brittle. The vendors implement the DICOM standard differently, sometimes it’ll pull up the wrong comparison image, etc. Radiologists waste a lot of time fixing these issues and setting up the images in the way they prefer to make a diagnosis. These seconds per case compound into hours per shift and higher cognitive load, and a workflow software can make a big difference.
A smarter worklist and viewer can automatically surface the most relevant prior, apply site- and modality-specific layouts with sensible presets, inline voice-to-structured dictation that pre-populates required fields and drops an impression scaffold in the radiologist’s style, and flag missing checklist items like laterality, comparison dates, and critical-result routing before sign-off. Basically making sure the images are loaded up right and to the radiologists individual workflow preference.
Plus, LLMs open the door to real-time documentation and reduce the amount of time docs need to spend writing. Wave 2 companies are leveraging generative AI to:
- Auto-compare to priors: pull the most relevant prior, then track each lesion as its own identity so baseline and growth are calculated per nodule (not averaged or mismatched). For example: “nodule 6 mm → 6 mm (0% since 2024-05-12, stable); LLL nodule 8 mm → 11 mm (+38% growth).” This cuts down time while preserving accuracy.
- Guideline-linked suggestion: when a 6 mm pulmonary nodule is described, propose a follow-up line consistent with Fleischner criteria for the documented risk profile, for radiologist approval. Because research evolves quickly, LLMs excel at surfacing and summarizing the latest findings.
- Style matching: learn a doctor’s preferred phrasing (“No acute intracranial hemorrhage” vs “No evidence of ICH”) and formatting, then draft in that voice automatically.
- Structured fields from voice: convert free dictation into discrete fields (e.g., BI-RADS category, LI-RADS features, fracture side/location) to drive consistency, QA, and downstream coding.
- Consistency checks: flag discordance between body and impression (body says “right,” impression says “left”) or between measurements and descriptors (“decreased size” but numbers increased).
- Site-aware templating: when reading for another hospital, auto-switch macros, exam names, and critical-result language to that institution’s standard without extra clicks.
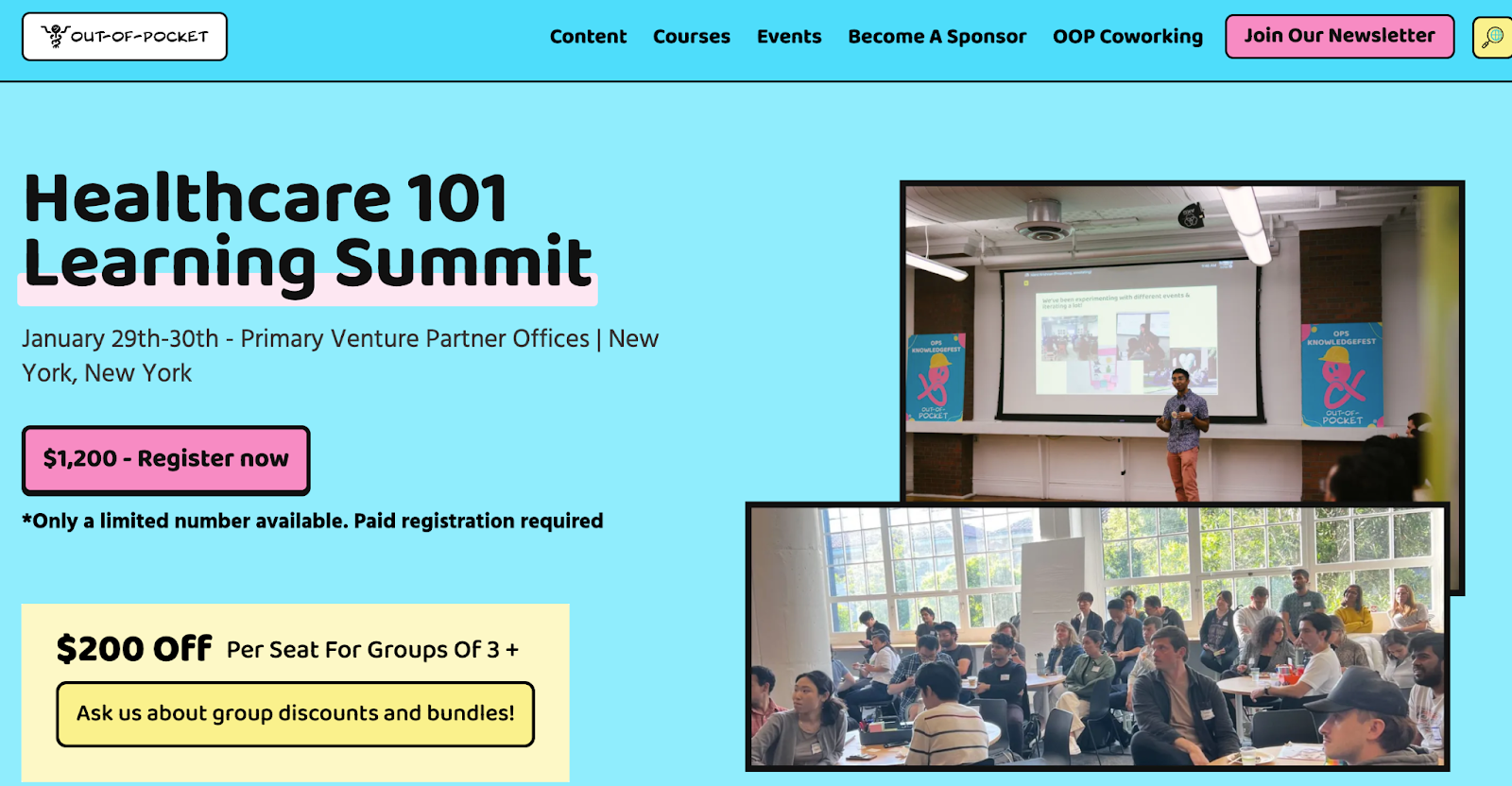
Quick Note - Healthcare Learning Summit, Limited Seats
We’re doing our Healthcare 101 Learning Summit in New York on 1/29 - 1/30! If you or your teammates are new to healthcare or need to learn about how the rest of the industry works, you should really come to this. Some people we tend to do well with:
- You have a bunch of people on your team that are from tech but new to healthcare and need to learn the ropes
- You’re launching a new product in a totally different part of healthcare and need to learn how it all fits together
- People at agencies, consulting, or finance firms with a healthcare division but no formal curriculum to learn how it works
- International companies or non-healthcare companies expanding into healthcare with a new product line
We have limited seats, so sign up sooner than later. Hit up sales@outofpocket.health for group sales.
And don’t forget we have a FREE course with Metriport coming about what data interoperability is, a buzzword you’ve probably heard many times.
Thanks to AI, people are more data hungry than ever. But what are the ways you can actually get data out of the healthcare system? We’ll talk about ways you can get data today, roadblocks to interoperability currently, and what’s changing. Come hang.
New companies are focused on improving training data
In the first wave of radiology AI, the lack of structured training data posed a significant barrier to progress. Clinical reports were typically written in free text, inconsistently formatted, and rarely linked to confirmed ground truth. As a result generating high-quality labeled datasets for training ML models required extensive input from radiologists. In many cases, we paid radiologists up to $250 per hour to manually annotate reports - expensive and tough to scale as you might imagine.
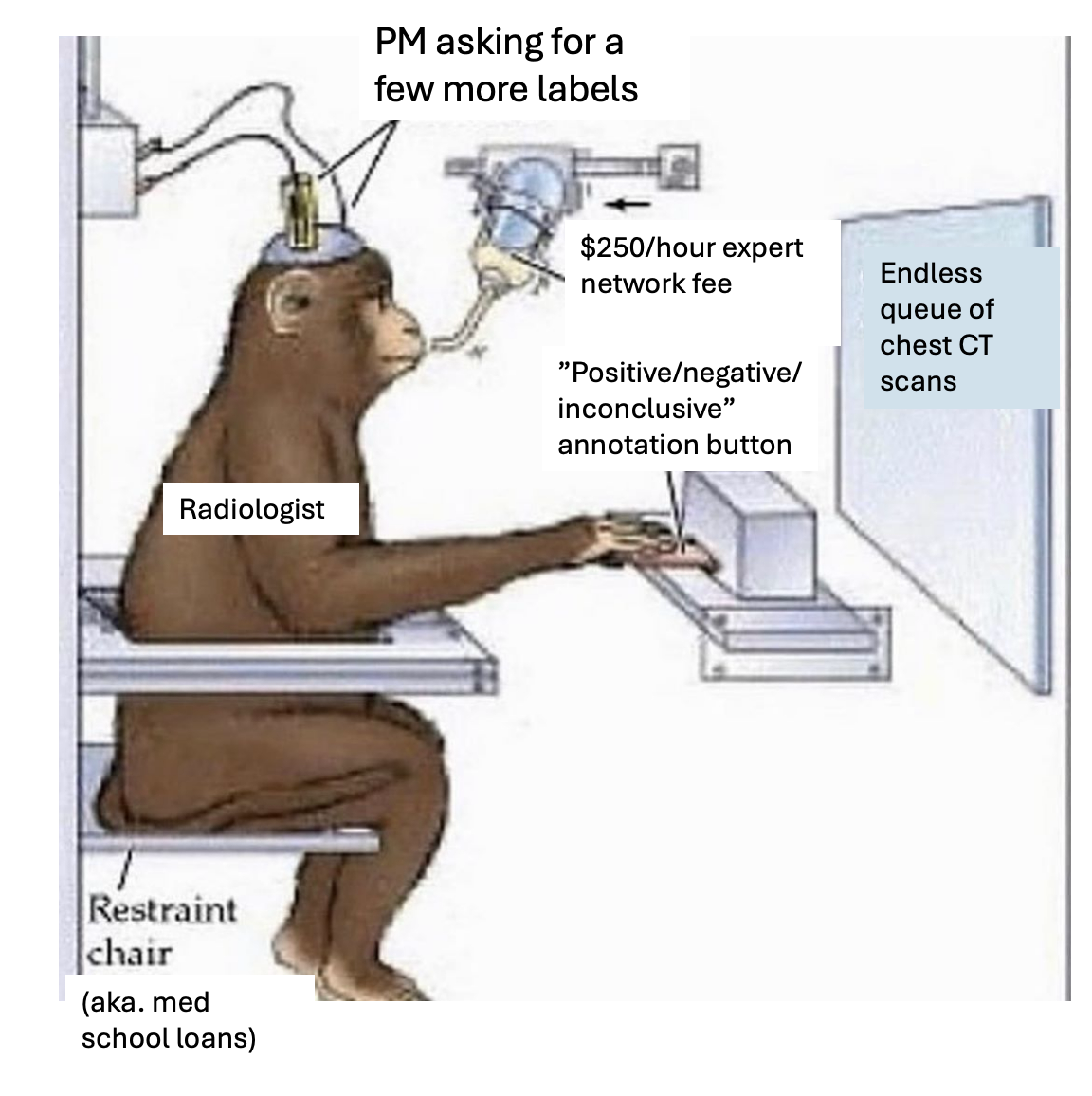
While LLMs don’t solve ground truth, they make it far faster to turn existing data into high quality training sets. They help by:
- Extracting structured findings from free text reports
- Segmenting imaging studies by anatomical or diagnostic relevance
- Pre labeling large batches of cases for clinician review
- Linking across modalities so related findings surface together
Until recently, building an imaging dataset meant sending every case to a radiologist and having them label it from scratch. A five thousand case CT project could take months because each case required full volume review, manual measurement, and structured transcription.
Today the workflow is faster. Models can scan the same five thousand studies, identify candidate findings, cluster similar cases, and draft initial labels. Radiologists only correct and refine these outputs.
Clinicians are no longer the primary labelers. They are supervisors who check, adjust, and validate machine drafted annotations. This shift cuts annotation effort by an order of magnitude while improving consistency and accelerating model development.
Using AI to expand imaging reads
Sometimes when you get a scan for one thing, you discover another medical issue in the process. But radiologists understandably aren’t looking for every single issue that could potentially show up on every image. New AI tools focused on workflow are surfacing issues within the existing images.
For example preventive reads like bone density signals on routine chest CTs can be auto-surfaced. Radiologists can catch other issues, patients get flagged for certain things they’re at-risk for, and hospitals capture the downstream revenue of other flagged issues. This also improves the sale to the hospital.
It’s also possible that the WHERE you get these imaging reads done expands as well. With workflow-first platforms, primary care and urgent care sites can stand up on-site imaging programs that bundle equipment, AI triage/QA, and remote radiologists for final reads. Some Wave 2 companies are pursuing this turnkey model, so non-radiology settings can triage and manage straightforward studies on site with AI-assisted workflows and teleradiology coverage.
This increases the number of image reads that can get done and reserving subspecialty time for the toughest cases (both of which are good for hospital sales).
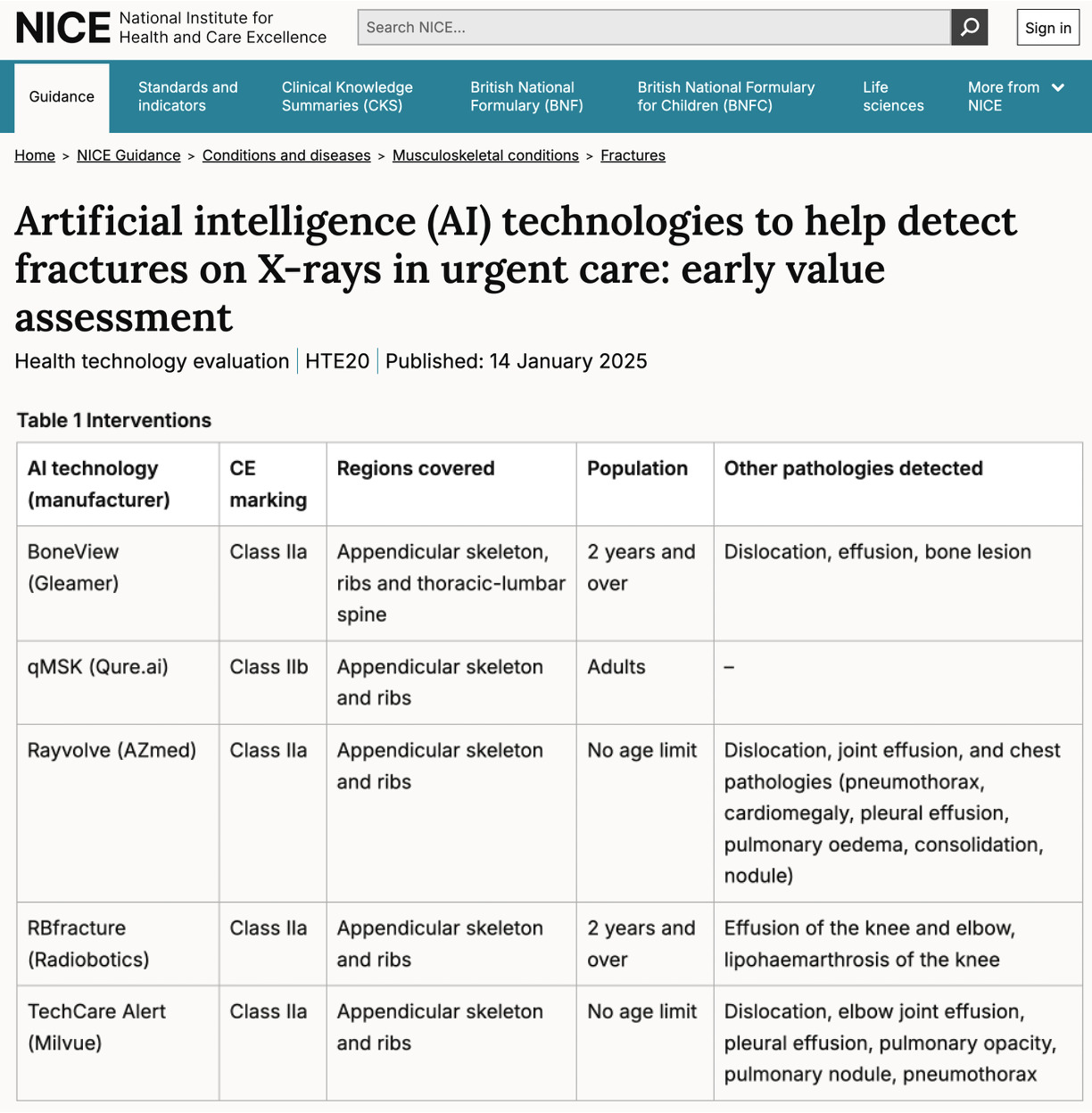
[NK note: AI in urgent care is an area that the UK seems to be exploring more deeply and testing over the next few years]
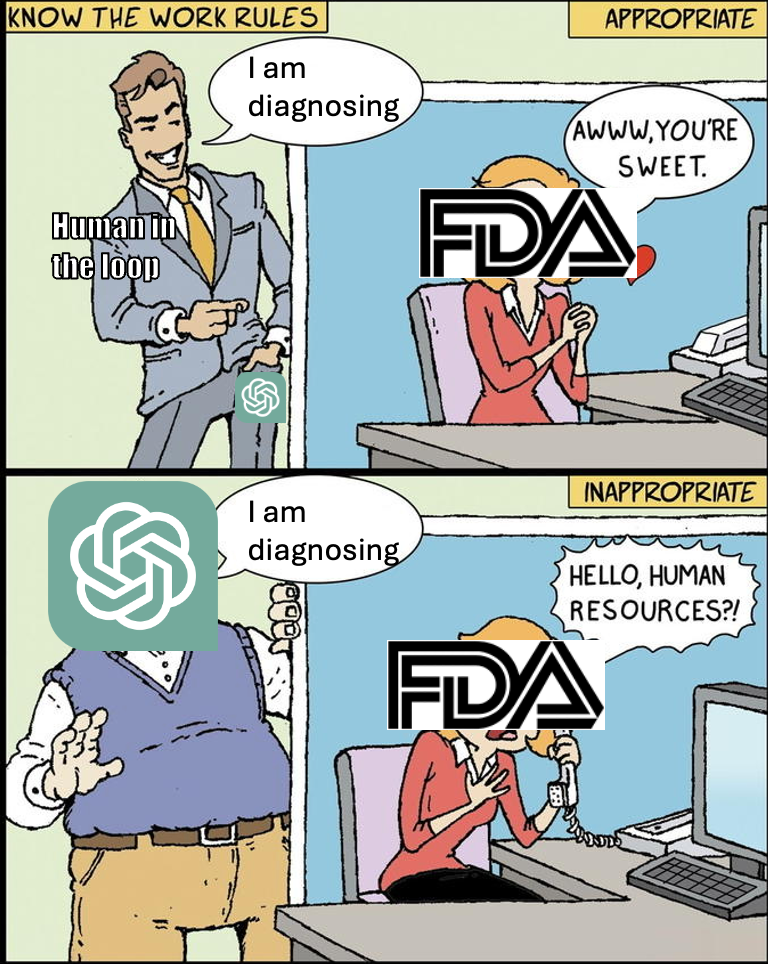
Clearer FDA requirements
Regulation and payment were brick walls for Wave 1; they are now navigable with defined on-ramps. The FDA has formalized pathways for iterative AI/ML including Predetermined Change Control Plans (PCCPs) that let sponsors pre-specify model updates (e.g. scope, validation methods, and impact assessment).
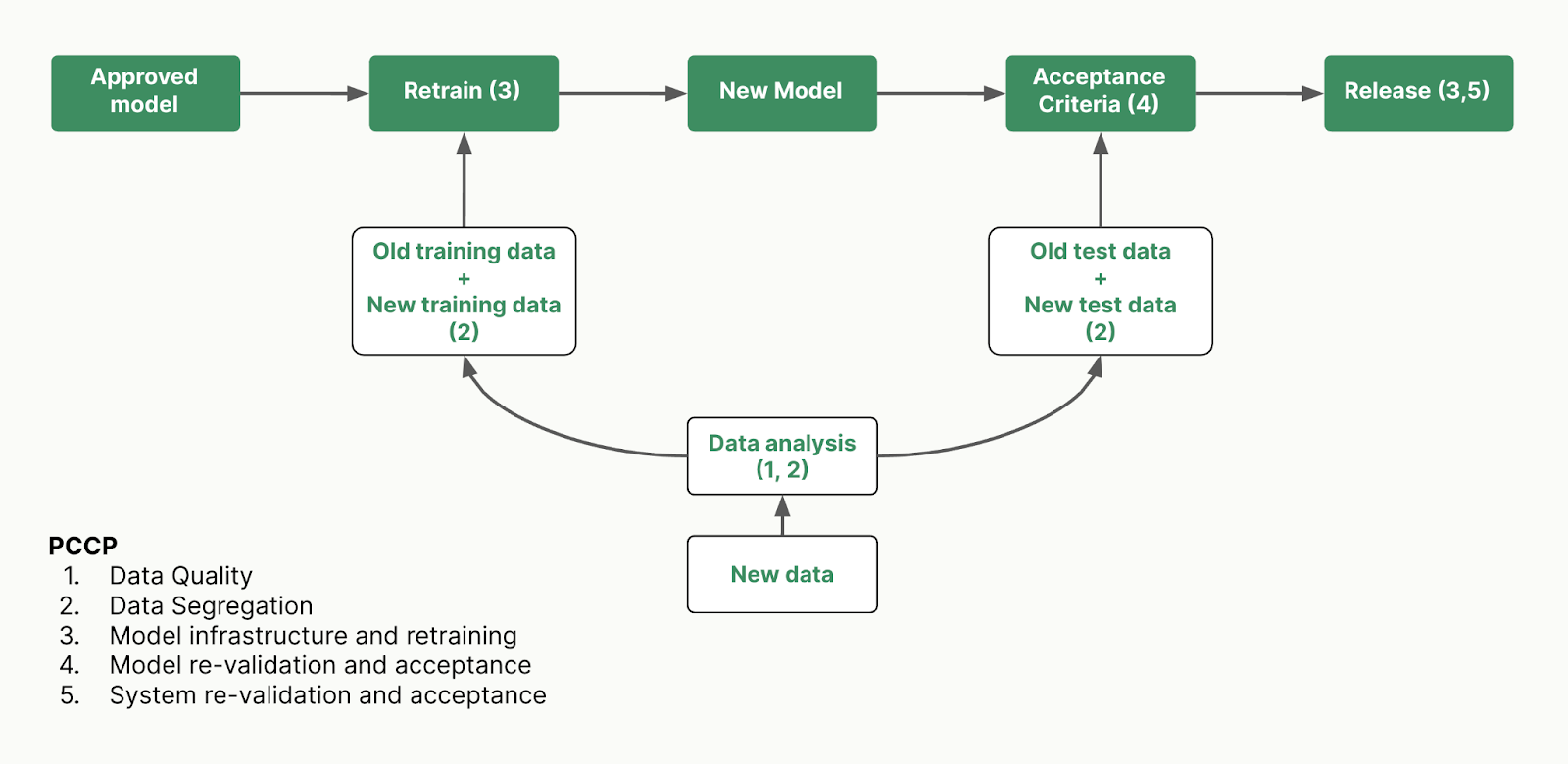
This means that routine modifications no longer trigger new reviews. Reader studies, real-world performance plans, and Good Machine Learning Practice (GMLP) expectations are documented and predictable rather than ad hoc.
However it’s worth noting that even with a clearer FDA pathway, reimbursement for these AI reads still is relatively limited. But the groundwork is being laid for getting approvals faster and setting realistic expectations for software companies operating in the real-world. We can see the recent reimbursement for AI coronary plaque analysis as a leading indicator here.
AI Is Embedded in Radiology Services vs. Sold as Standalone Software
The next generation of radiology AI companies are moving away from selling isolated point solutions. Instead, they are embedding AI within end-to-end radiology services, offering radiology-as-a-service, automated impression generation, clinical documentation, and quality assurance systems that flag potential errors in real time.
When you sell workflow instead of a point algorithm, you change how you sell to hospitals. Instead of onboarding a new vendor and going through IT, compliance, and legal each time the buyer can evaluate one platform that sits in PACS/dictation and covers the full imaging workflow. That means a single BAA and security review, one set of integrations, one MSA, and expansion by SOW. No fresh RFP needed every time you add a feature.
The reality is that hospitals don’t want a standalone tool for wrist fractures, another for pneumothorax, and a third for bone age. The procurement, integration, and training burden makes that model unsustainable. Platforms gets budget through existing radiology operations or teleradiology contracts and they show their value through throughput, turnaround time, report quality, and denial reduction. The additional AI modules in the platform can just ride the same rails without reopening purchasing.
This shift reflects a deeper strategy: instead of layering AI onto someone else’s workflow, these companies are building and operating the entire stack. Everything from image acquisition through report generation and billing. In some cases, this has meant acquiring radiology groups or integrating with large practice networks.
At Nines we recognized early that hospitals weren’t necessarily looking for more software vendors. They were looking for outcome-aligned partners. We initially built an FDA-cleared triage model, but soon pivoted from SaaS to service delivery by acquiring a radiology group and offering AI-enabled reads. This allowed us to align more closely with hospital budget structures: instead of charging software subscriptions for our AI tools, we charged teleradiology prices where AI-enabled efficiencies were baked into the delivery.
But this strategy comes with tradeoffs. Operating a radiology practice is enormously complex (e.g. managing 24/7 coverage, staffing variability, licensing, malpractice, and shift allocation). Mega-groups may be better positioned to pursue this model because they can leverage economies of scale and route studies across a national pool of radiologists. But even they find that squeezing margin out of radiologist workflows is limited, even with AI in the loop.
So why are Wave 2 companies pursuing this model today? A few reasons:
- You can build totally new workflows by bundling a lot of these incremental AI workflow improvements if you own the practice
- You can tap into the headcount and professional services budgets at hospitals, which are much larger than tech budgets.
- You can bypass the need to get every AI assistance FDA approved, and instead have a human in the loop.
- If you believe you can materially improve patient outcomes with your tool, you can eventually change your contracting so you participate in the upside.
But operating a practice is not for the faint of heart, and is much more about everything that’s not the technology itself.
The Open Questions Here
While I’m optimistic about the future of AI in radiology, there are some open questions that will dictate what the future of this space looks like.
- Will radiologists trust AI assistance if it’s not FDA approved? And how foolproof does the AI need to be before radiologists trust it? If the radiologist needs to constantly double check the AI then the workflow efficiencies basically get eliminated.
- Relatedly, where will liability end up shifting? Part of the reason the radiologist needs to double check everything is because they’re the ones that take on the risk. Will AI companies start competing and building trust by absorbing liability? Will new insurance products for AI tools become popular (e.g. AIUC)?
- How far are we from fully autonomous reads for simple cases? If teleradiology practices can shift simple cases to full autonomy it changes the practice economics significantly. Or It can enable some of these non-radiology sites of care to expand the number of cases they can triage.
- If you increase the throughput significantly with these AI reads, is there capacity on the hospital services side to handle that?
- One issue with value-based care in radiology is that you need to link the rest of the patient journey to see how costs actually changed downstream. With better linkage/interoperability, will we see meaningful changes in contracts that are tied to downstream pricing vs. focusing on increasing fee-for-service throughput at practices?
Featured Job Postings
A few companies are hiring now!
Percepta (Applied AI engineer - Multiple Locations)
- Build the AI transformation playbook for U.S. healthcare. Full ownership of Summa Health (via GC) = huge access to ship production agents across clinical & ops workflows. What we prove here will expand nationwide. Apply here.
Percepta (Data engineer - Multiple Locations)
- Build the data infrastructure playbook for AI in U.S. healthcare. Full ownership of Summa Health (via GC) = huge access to Epic, claims & clinical data to power agents at scale. What we prove here will expand nationwide. Apply here.
Mending (Product Engineer - NYC/Remote)
- Mending is hiring software engineers (hybrid in NYC or remote in the US) to help doctors focus on delivering care instead of paperwork. Mending insurance products bring innovative payment models like Direct Primary Care to more patients and more employers. Apply here.
The final takeaways
For the readers who were going to run this post through ChatGPT, here’s a cheat sheet that summarizes my experience in AI + Radiology:
- Sell results, AI is secondary - No one wants a model. Everyone wants fewer hours worked, faster reads, fewer errors, higher reimbursement.
- Disappear into workflow - AI tools must live inside PACS, work with dictation tools, and integrate with the EMR. New tabs and extra clicks are the headline of most healthtech obituaries.
- Point solutions are in for a bad time - Sorry to tell you this but if your tool solves one task, it’s a feature not a business.
- Data and workflows are the moat - You structured multimodal dataset, how fast you can refine it, and how that improves workflows are the actual moat. Experiment with synthetic data to strengthen and accelerate your model development.
- Don’t bet everything on FDA approval - The timelines are unclear and you need to stay afloat. Keep doctors in the loop to go to market faster and with less friction.
- Have a clear answer on business model - How much are you going to be paid, by whom, and from which budget?. What’s your pricing thesis? Your ROI story?

[NK note: It’s also clear how much of this is timing the market. Being a first mover in any AI category has seemingly been a mistake because no one understood how to reimburse it and you spent most of your time educating the market. The second mover advantage here is huge because of how much more mature the buyer and regulatory environment has become AND how much better the tech itself has become thanks to new foundation models.
Big thanks to Ayushi for putting these thoughts together.]
Thinksquad out,
Nikhil aka. “Hanging protocol? You mean cracking open a cold one?”
Ayushi aka. “I love studying radios”
This piece wouldn’t have been possible without insights from conversations with radiologists, ML engineers, healthcare operators, and my teammates at Nines. Thank you to Nikhil, Jan, Jaymo, Rebecca, Nand, Laura, Leora, Zach, Natasha, Abhijeet, Manvesh, Naina, and Astha for providing feedback.
Twitter: @nikillinit
IG: @outofpockethealth
Other posts: outofpocket.health/posts
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!!
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
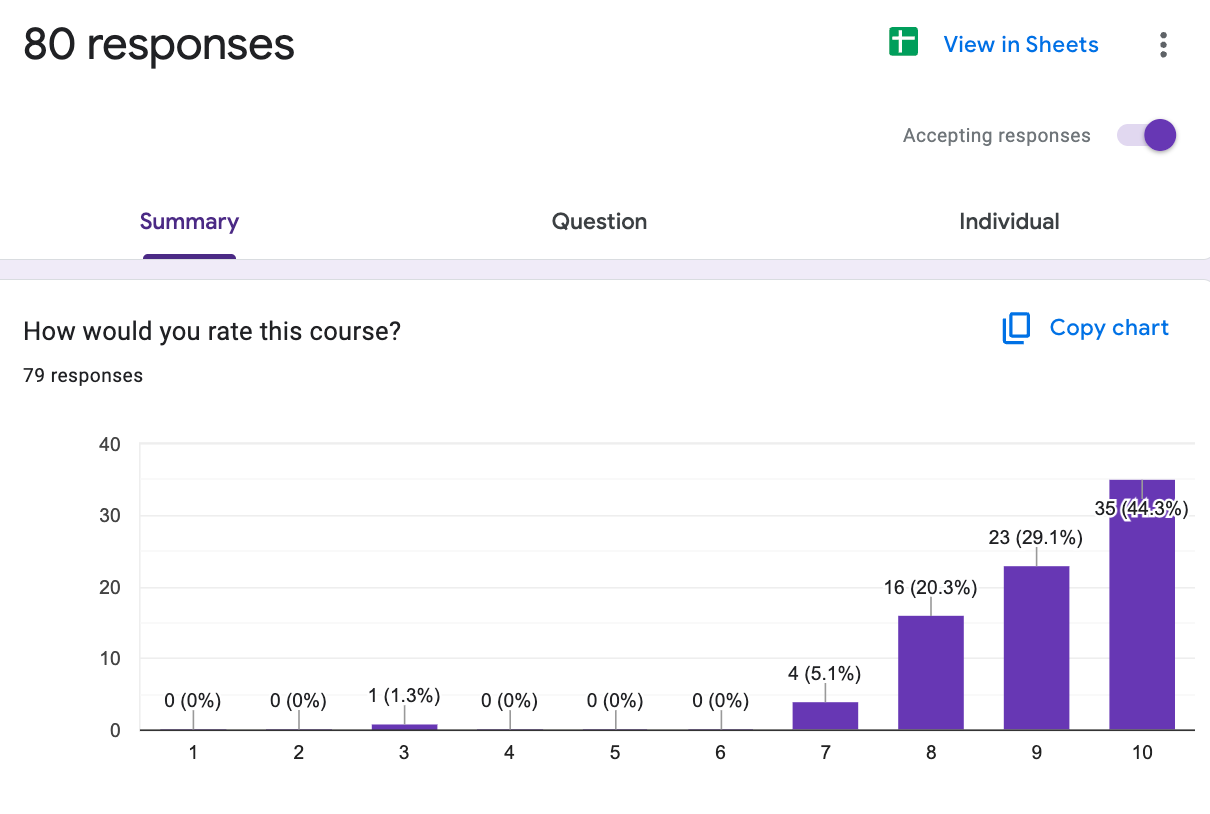
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!! And it’s the final run for all of them (except healthcare 101).
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
How to contract with Payers (starts 9/22) - We’ll teach you how to get in-network with payers, how to negotiate your rates, figure out your market, etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →A reminder that there’s a few courses STARTING VERY SOON!! And it’s the final run for all of them (except healthcare 101).
LLMs in healthcare (starts 9/8) - We break down the basics of Large Language Models like chatGPT, talk about what they can and can’t do in healthcare, and go through some real-world examples + prototyping exercises.
Healthcare 101 (starts 9/22) - I’ll teach you and your team how healthcare works. How everyone makes money, the big laws to know, trends affecting payers/pharma/etc.
How to contract with Payers (starts 9/22) - We’ll teach you how to get in-network with payers, how to negotiate your rates, figure out your market, etc.
Selling to Health Systems (starts 10/6) - Hopefully this post explained the perils of selling point solutions to hospitals. We’ll teach you how to sell to hospitals the right way.
EHR Data 101 (starts 10/14) - Hands on, practical introduction to working with data from electronic health record (EHR) systems, analyzing it, speaking caringly to it, etc.
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.
INTERLUDE - FEW COURSES STARTING VERY SOON!!
See All Courses →Our Healthcare 101 Learning Summit is in NY 1/29 - 1/30. If you or your team needs to get up to speed on healthcare quickly, you should come to this. We'll teach you everything you need to know about the different players in healthcare, how they make money, rules they need to abide by, etc.
Sign up closes on 1/21!!!
We’ll do group rates, custom workshops, etc. - email sales@outofpocket.health and we’ll send you details.

Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







