2026 Healthcare Predictions Part 2
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
This episode of Out-Of-Pocket is brought to you by…
At AndHealth, we believe healthcare is a human right. We're focused on expanding access to specialty care, specialty pharmacy, and improving health outcomes for chronically ill & medically underserved populations.
Explore opportunities to join our team!
—
We ain’t out of office anymore!!!
Last week I talked about some predictions I had for 2026. Many of you replied saying “OOO – I’m traveling until 1 / 5”. To those people I say…enjoy my schedule send emails coming in hot at 8AM.
But the rest of you are like me - thinking about healthcare on New Year’s even, using the countdown to think about my deductible resetting. Those people sent in some of their 2026 predictions.
My favorites below, memes and comments from me.
Direct contracts in response to the uninsured rate
“As the uninsured rate climbs (as a result of HR1 and the expiration of enhanced subsidies), hospitals will likely see a spike in bad debt and collections burdens. Paired with the rise of high-deductible plans, this creates a nightmare-like scenario for providers on the collections front. At the same time, employers are pushing for favorable deals through direct contracting (a notable effort is Cost Plus Wellness, a network built by Mark Cuban’s Cost Plus company).
Offering lower rates may seem like a loss for providers, but there are elements of direct contracts that can benefit them, such as 0% cost-sharing and deductible carve-outs. Community hospitals and small health systems may start entertaining these arrangements more seriously; negotiating a direct contract with a large local employer can create guarantees around volume and price that provide greater certainty. Large health systems may not play ball with aggressively priced direct contracts, but negotiating carve-outs (on deductibles, etc.) and renegotiating contract terms will certainly be on the table.”

[NK note: I’ve been hearing “direct contracting is about to take off” for as long as I’ve heard “Hudson Yards is about to pop off”. All of the arguments seem logical especially around collections, but I just don’t think employers want to take on that burden. I was at a self-funding conference last year where someone talked about this - and it’s basically someone’s full time job to manage these contracts.
But hey…maybe 2026 is actually the year for Hudson Yards.]
Quick reminder - Healthcare 101 Learning Summit + Free Interoperability course!
Quick reminder - our Healthcare 101 Learning Summit is on 1/29-1/30 in New York. ENROLLMENT ENDS 1/21!
We’ll teach you how healthcare works, how the money flows, have guest lectures with real world case studies, and you’ll meet a bunch of other cool people in healthcare. Ping sales@outofpocket.health for group rates.

And a reminder that our FREE interoperability course with Metriport starts 1/20-1/22. We’ll talk about all the changes in interop rules for 2026, what the state of pulling healthcare data looks like today, and more. If you need to pull in healthcare data for your business, you should come to this. Plus we always have a poppin chat where people give their own perspectives, and it’s FREEEEEEE.
The Medicare Advantage Prior Auth Experience Arrives in Traditional Medicare
“As CMS progresses towards ubiquitous value-based care in Medicare, the core vehicles are MA and CMMI pilot programs operating in Medicare FFS. Historically, CMMI programs introduced VBC features, e.g. risk adjustment, quality measurement and prospective capitation. These incentives are operationalized behind the scenes as EHR alerts and care gap spreadsheets. Patients only notice rising prices and the harried look of clinicians.
In 2026, CMMI’s WISeR model revises Medicare FFS’s minimally invasive prior authorization program. It kicks off a five year bake-off where prior authorization vendors (many already servicing commercial insurers) conduct prior auth for a limited set of services in limited geographies. The scope of the program today focuses on FFS fraud hot-spots (think $10B in skin grafts) which were largely averted in MA due to prior auth programs. Importantly, CMMI explicitly states it can expand the geographic scope and / or service categories of the program with each assessment of its effectiveness. Since effectiveness = spend reduction and the same processes are well-tested in MA, the space of providers with effective “gold cards” will probably go down over time.
Back to the patient UX which varies dramatically across MA and FFS. A KFF study of 2023 period estimates 1.8 PA determinations per MA enrollee vs. 0.1 in FFS. In 2026, a much wider swath of FFS beneficiaries will be exposed to the workflow below.
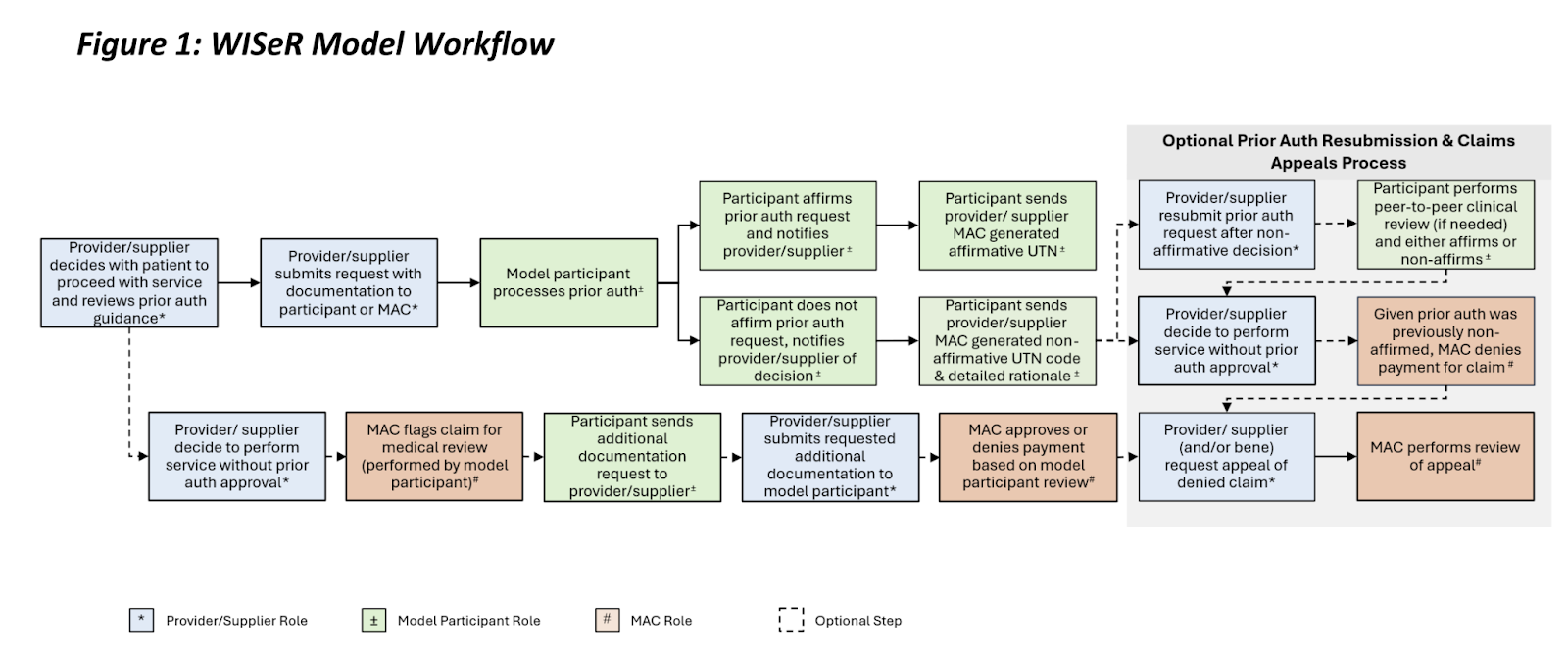
Not pictured is the anxious patient or caregiver who unclogs the process by:
- Calling all three parties involved
- Learning someone is pointing at someone else
- Consulting GPT / friend who works in healthcare
- Resolving the confusion
- Service is denied anyway
- Commences next iteration of workflow
To be fair to CMS and insurers, this is a super hard problem. A balanced program which averts fraud without driving clinicians and patients crazy remains elusive. My sense is FFS patients are not going to be enthused though.
To learn more, I recommend Sidney Menack’s write up and the CRS Report as starting points.”
[NK note: I feel like one of the big reasons that people who turn 65 choose traditional Medicare is to be able to see any doctor they want and not deal with utilization management runarounds like prior authorization. I wonder if this is actually going to change how older people make the decision between them - or if the scope is still too small for it to matter since it’s only a handful of specific a shortlist of procedures it applies to.
GLP-1s - the king stays king
“Predictions for GLP1 (in weight loss) we can look back and verify somewhat:
> 50% of patients starting GLP1s under insurance in 2026 will be enrolled with a lifestyle program. And > 50% of patients starting a GLP1 in 2026 will be cash pay DTC.
Employers want to restrict GLP1s (via peterson institute, Dec 2025) because, you know, they like money (patient persistence also growing). The easiest (morally and feasibility) is just require a lifestyle intervention + GLP1 with evidence of ongoing benefit. CMS has signaled a similar strategy offering lifestyle interventions with GLP1 coverage
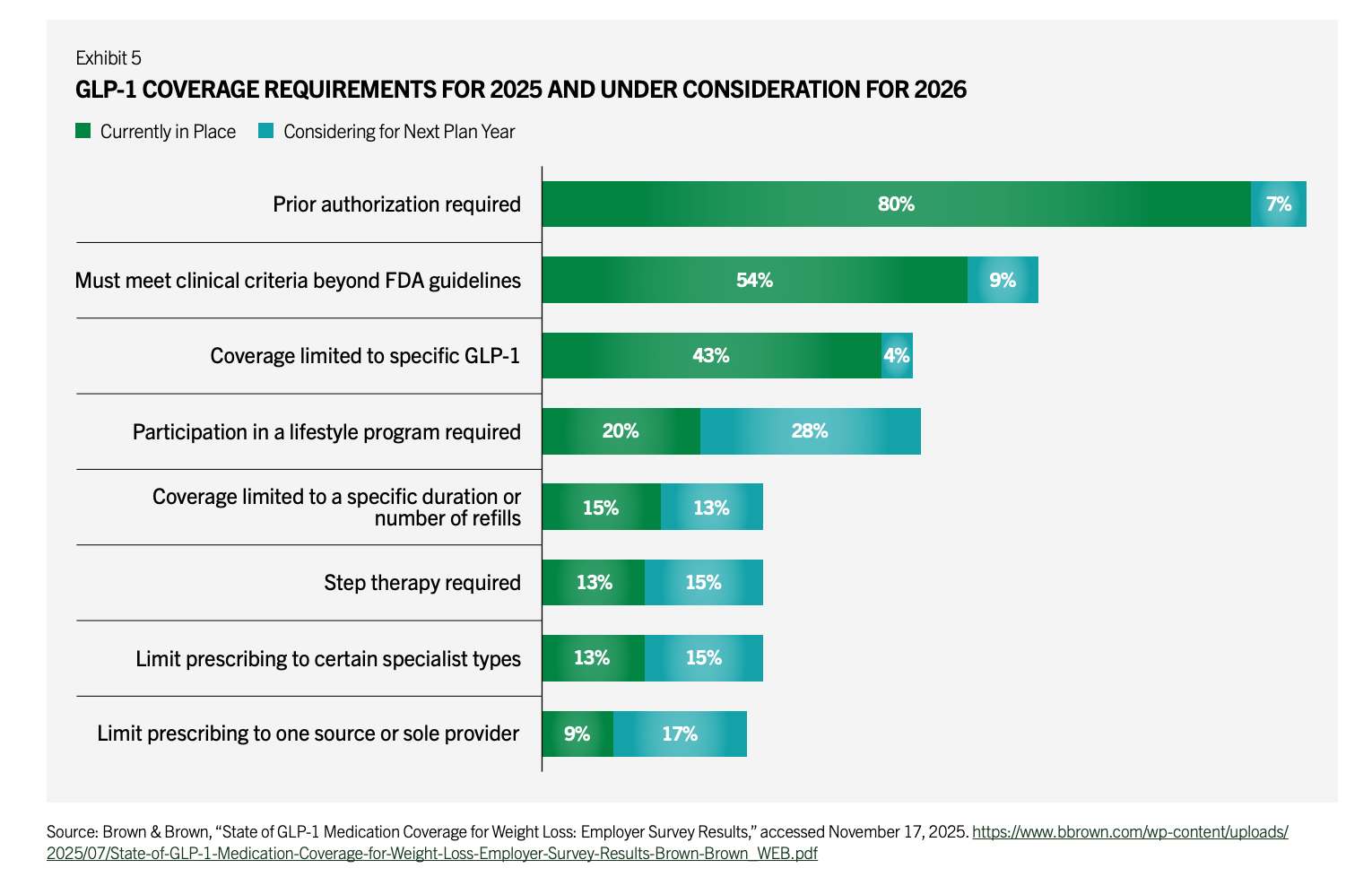
10% of wegovy, 30% of zepbound is cash pay right now. Now imagine there's an oral Wegovy (approved) and an oral GLP-1 (orfoglipron) - 150/month on < 200/month through Novo direct/TrumpRx for pretty much a maintenance dose of the medication.
And all the nonsense with compounding pharmacies? Yea, They're cooked According to Novo, 1 million patients are on compounded GLPs but imo this could be < 200k by EOY as customers realize it's the same price from Lilly/Novo. HIMS is not Him.
Putting these together, I will make the same prediction I made before: the king stays the king. A few new mechanisms (Amylin, triple G (is that a wrestler?), myostatin (to get f***ing jacked), INHBE for longer dosing, etc). Amylin is the only one with a chance because of better tolerability. Tirzepatide is the King: the solution is GLP1/GIP + lifestyle + Lower dose/Oral for maintenance.
Side note: LLY will likely outspend the NIH next year for their focus Areas (Cardiometabolic, immunology, Neuro, Onc)”
[NK note: HIMS is not him is a bar. That’s all.
One issue if 50% of GLP-1 users are actually cash pay is that this is going to be a nightmare for anyone that relies on pharmacy claims data to do anything. Plus I feel like we’re actually missing out on some interesting analyses on whether patients are seeing improvements in other disease areas]
The Medicaid doom loop increases government dependence
“HR1's Medicaid cuts will ironically make healthcare MORE dependent on government payments, not less.
When you cut Medicaid payments, already-distressed hospitals close first. They're running on thin margins and can't absorb the revenue loss. Loss-leading service lines (pediatrics, OB, behavioral health, etc.) shut down first.
But Medicaid patients don't vanish. They concentrate at the remaining providers - typically large academic medical centers AMCs that can't refuse them (EMTALA, mission, political leverage).
This creates a doom loop: The survivors see their Medicaid payer mix increase just as per-patient revenue decreases. They become MORE dependent on supplemental payments at exactly the moment those payments are being capped.
It's like closing county roads to save on maintenance costs. Traffic doesn't disappear - it just concentrates on the interstate, which now needs MORE funding for repairs and expansion, not less.
It's happened before: states cut Disproportionate Share Hospitals DSH payments in the 90s to force AMCs to become more efficient. Instead, smaller safety-net hospitals closed or consolidated, concentrating Medicaid volume at major teaching hospitals.
The policy tries to cut government healthcare spending. But cutting Medicaid makes survivors more dependent on government revenue, not less.”
[NK note: The open question here is whether programs are used to float hospitals that will be most hit by Medicaid cuts (e.g. the new rural health fund). My sense is that there’s a dance in trying to create policies that help struggling hospitals in lower resource areas while also not having those programs abused by larger hospitals. But I’m not really a policy guy.
I do feel for these smaller hospitals that serve their communities with upside down economics who are caught in the crossfire.]
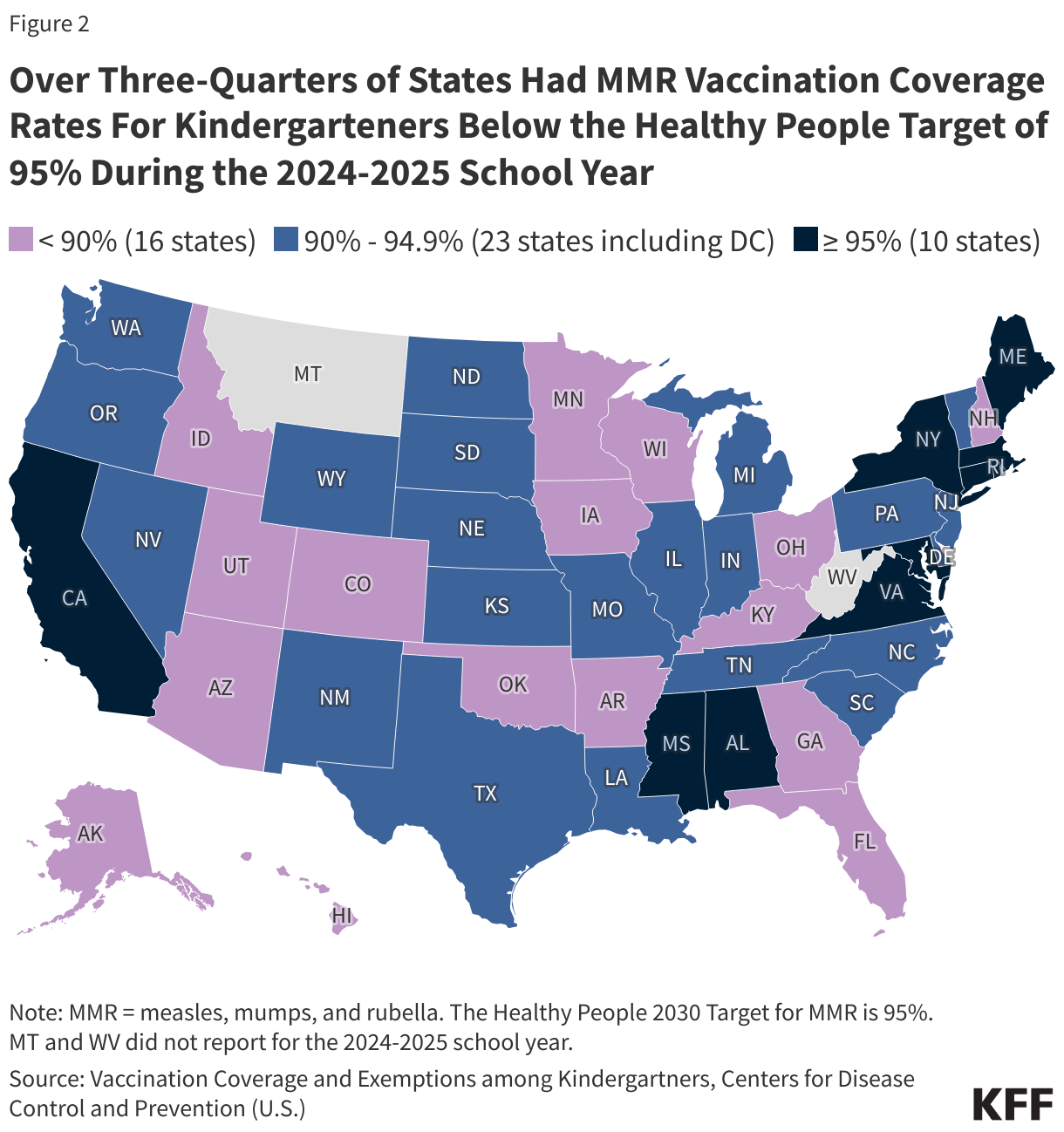
Vaccines are…back?
“Spurred by several nationally documented outbreaks (e.g., a mother who tested negative, decided against vaccination but passed on Hep B to their newborn), some states see vaccination rates increase as people realise that “maybe vaccines weren’t so bad after all.” That shift creates clearer demand signals, attracting more private capital into vaccine R&D even without new public funding.
Given COVID‑19’s recency bias, mRNA vaccines remain contentious; however, views become more balanced as lived experiences on both sides enable a clearer “compare the pair,” reducing the dominance of low‑incidence adverse event anecdotes. Even if guidelines soften further, uptake ticks up in areas affected by recent outbreaks. The net effect is a grassroots, apolitical pro‑vaccine push based on observed benefits rather than ideology.”
[NK note: As much as I’d like this to be true, there are already lots of documented outbreaks and I don’t think that’s changed many people’s minds. The issue is that this will be met with as many anecdotes on social media that confirm whatever your pre-existing belief is.
I’m really not sure how to re-establish trust in well-studied vaccines, but would love to hear more ideas.]
Featured Jobs
Weeeee got some companies hiring!
Chamber: Provider Success Manager (Washington DC, Remote)
- We’re looking for a Provider Success Manager to serve as the front-line partner for our network practices. You’ll work directly with physicians, practice managers, and care teams to help them thrive in value-based care — driving clinical performance, optimizing technology adoption, and ensuring the success of each practice under Chamber’s model.
Bonfire Analytics: Data Analyst, Customer Success Healthcare (New York, NY)
- Bonfire helps healthtech companies accelerate their GTM selling into healthcare providers/organizations. If you have passion and curiosity for working with messy healthcare data and managing customer relationships, join us as employee #7! Apply here.
Immunera: Principal Machine Learning Engineer (NY/Hybrid)
- Bring language models to the clinic: Immunera builds blood tests powered by gene sequencing and protein LLMs. Our tech is published in Science and covered by NYT & STAT. We’re hiring a Principal ML Engineer to lead the models and infrastructure behind our first autoimmune disease test. Get in touch.
Resetting of wearables regulation
“Lots of pressure from companies to de-regulate wearables -- see this WSJ op-ed from Oura Ring CEO, this fight from Whoop over the FDA's warning letter. Companies like Apple have sought to embrace regulation as a competitive moat for products like the Apple Watch, whereas their competitors are fighting for de-regulation to compete in what they perceive is a consumer market. New tailwind now with the CMS ACCESS + FDA TEMPO model, which will further add pressure to change how we regulate these technologies.
Fits nicely with the tailwind you called out about increased flexibility for patients to use products (in the case of your prediction email, point-of-care testing) at home.
Why does this matter? Because the current administration loves wearable tech (see this nice Atlantic piece on MAHA + CGMs), the tech frankly is innovating quite quickly, there is a huge market opportunity (with nice integrations with care delivery / VBC models), and regulation for medical devices has always been more of a wild west than it has been for drugs.
Is this a good thing? Maybe -- it is kind of remarkable what these devices can do, and the fact that consumers willingly adopt them (unlike most things in healthcare) says a lot about their potential. But there are of course risks; especially if devices with less-than-ideal performance gain traction (with risks for both false positive / false negative results).”
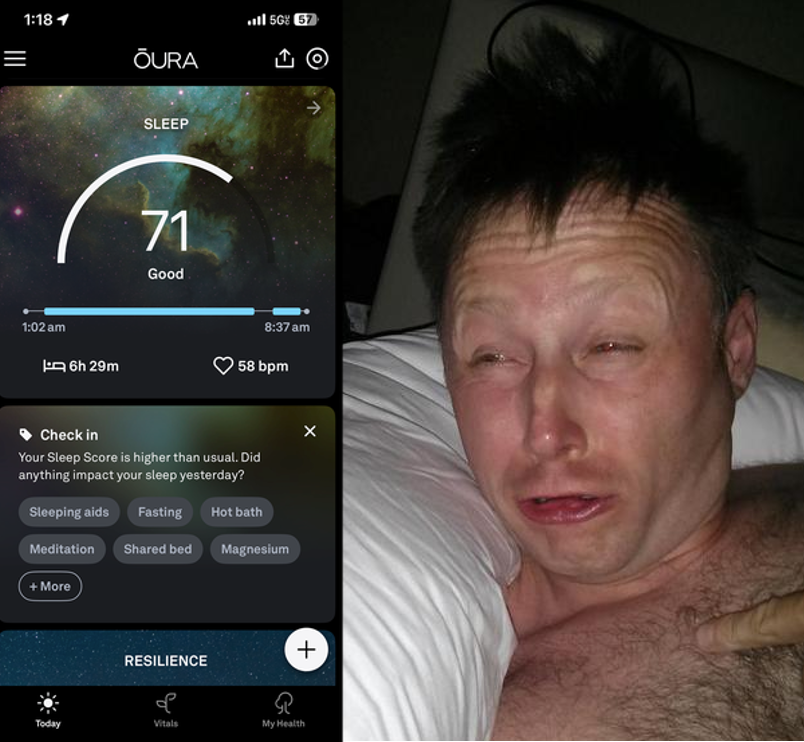
[NK note: I like this one, and at Out-Of-Pocket we’re also betting wearables are going to become a bigger part of healthcare (which is why we’re doing our hardware hackathon in April in SF!).
The question is what care protocols look like in a scenario where wearables are the front door. How you think about triaging, notifying patients of issues, doing telemedicine, routing, etc. will look extremely different if a wearable is the first touchpoint. Especially if you need to be weeding out the false positives when a bunch of healthier people are wearing these.]
Scribe -> AI agents
“After a massive wave of funding into AI Scribes (>$1B in venture capital over the past ~3 years including ~$800M raised in 2024 alone). There are some big names (Abridge, Suki, Nabla, Heidi), and now Epic is entering the AI Scribe market. We’re seeing prices dropping - from an initial average of ~$100/month for a D2C scribe to $60-70/month. Now there are more than +60 scribes available.
AI is undoubtedly unlocking huge value in healthcare which is proving to be one of the fastest adopting industries. The trouble with the initial wave of models is they are targeting the obvious stuff, with minimal to no barriers to entry. So we’re seeing spectacular growth curves, lofty valuations, and then margins and valuations plummeting on functionally commoditized products. If 2025 was the year of the AI Scribe, is 2026 the year of the AI Agent for Live Calls (Hello Patient, Assort Health, etc.)”
[NK note: I kinda think all of these areas start merging. Agents, scribes, clinical decision support, etc. will all start blending because end-to-end workflows need each of those pieces. You’ll probably see mergers, partnerships, etc. in this area.
The real fight is going to be between the companies that optimize for B2B use cases vs. consumer experience. This is going to have a lot of impact on how companies choose pricing, which I think will generally move towards some form of usage based pricing that’s dependent on number of features.
The analog here would be cloud providers, which are also sort of commoditized but differentiate on different workflows and tools on top of them. And they have usage-based billing, features that increase the pricing, and managed services.]
The White House boosts biotech
The White House will launch a “CHIPS Act for biotech” initiative, anchored by an Executive Order and/or HHS/FDA directives, explicitly framed around beating China on speed-to-clinic. The motivation: China is now surpassing the U.S. in many key areas of biotech, especially early-stage clinical trials, and the U.S. doesn’t want biotech to repeat the history of industrial manufacturing or rare earths (innovated here, industrialized elsewhere, then rediscovered as a national-security vulnerability).

The EO/directives will lay out a plan across multiple government agencies to compress drug development timelines and build clinical trial and manufacturing capacity, including:
- Speed targets for IND→first-patient dosed and site activation timelines, with public scorecards and agency accountability.
- A streamlined/lighter touch IND pathway for low-risk first-in-human studies, with less onerous requirements closer to peer countries like Australia, allowing preclinical biotechs to get to clinical PoC faster and pushing more US biotechs to run their trials here vs internationally.
- FDA “fast lanes” for early clinical (first-in-human + early PoC): more high-touch review, standardized submission templates, faster protocol amendments, and expanded use of master protocols/platform trials.
- A pre-qualified national site network with activation SLAs (and a public directory), so sponsors can “plug in” to sites that are ready-to-run.
- Trial-data plumbing modernization (interoperability requirements, common data models, etc) to accelerate multi-site studies.
- Patient enrollment incentives, e.g., travel/lodging support, paid time off stipends, and standardized compensation guidance, to reduce friction and accelerate recruitment and retention, especially for Phase 1/2 studies.
- Industrial base incentives for “Phase 1-ready” GMP capacity and critical inputs (plus faster facility permitting where possible).
- Trusted vendor certification (Know Your CRO/CMO/CDMO) tied to supply-chain security and federal contracting eligibility.
[NK note: People are very worried that the US is going to let biotech get offshored to China the same way manufacturing did. I enjoyed Alex Telford’s post about why this happened:
“But probably the most important change was slashing clinical trial start-up times, especially for first-in-human (phase I) trials. Before companies can test their drugs in humans, they need to submit an IND application to their country regulator. The Chinese IND process was slow and burdensome, regularly taking over a year for approval. The CFDA shifted to an “implied license” approval system for clinical trials in 2018 — if regulators didn’t raise concerns within 60 days of an IND, companies could proceed. As a result of the reforms, the average time for IND approval dropped from 501 days before the reforms to just 87 days after.”
I agree the US will probably not want to lose our pharma dominance. I think we’ll see the FDA push things like allowing real-world evidence to be used in trials (e.g. external control arms) and more interesting trial designs (e.g. adaptive platform trials). I’ve been enjoying reading some of the suggestions from the Clinical Trial Abundance people]
Bad thing in healthcare AI + consumers get medical-grade AI
1) Building on this one -- I think the first "bad thing" related to healthcare AI happens this year. That could be either:
- A data breach, like a vendor leaking sensitive data or PHI through prompts
- A doctor uses ChatGPT on their personal account (vs. enterprise) and PHI gets leaked (or shared publicly through that share button)
- A decision support tool like Open Evidence / Doximity GPT suggests something incorrect to a clinician (because of the LLMs are stochastic) --> a very bad thing happens to the patient
In response, a lot of systems will put the clamps on their providers' usage of AI -- especially the myriad free tools that exist.
2) I think that consumers will increasingly demand access to the same "medical-grade" AI that providers now use. When I am sick, I go to OpenEvidence to try to understand what's wrong with me (they allow a few free chats before forcing you to sign in and prove you're a doctor). When one family member got the flu last week + someone suggested we take tamiflu preventatively, I thought they were nuts and fact-checked them (on OpenEvidence of course) - only to find that taking tamiflu after exposure substantially reduces the likelihood and severity of symptoms (though public health hardos might not like that).
I am a nerd and want the expert grade knowledge (which can be dumbed down infinitely) rather than getting foiled on health searches on google/chatgpt/claude. I think many folks have similar preferences to me, and I also think that the risk of "misinformation" (or broken user trust) is lower because of how people interact with genai tools today: they hallucinated so much a few years ago that there's an implied "caveat emptor" (verify everything, there is a chance it could be made up).
- Anonymous
[NK note: It will be a shame if we allow a handful of bad, public stories to dictate how we use AI in healthcare. Regulations that get put up to deal with those stories will only favor incumbents.
re: Medical grade AI, I’d be curious how many areas where there are deltas between responses that the doctorGPT gives vs. regular chatGPT. If anything I would expect the consumer LLMs to be more willing to give less “verified” but interesting responses vs. the doctorGPT which is likely MORE guardrailed]
D2C pharma works and expands
My prediction is that the direct-to-consumer strategy for Ozempic/Mounjaro and the like is going to be so successful that new, non-GLP1 drugs will start their own direct-to-consumer ordering programs and bypass pharmacies. Complex drugs that involve REMS programs and ongoing labs for monitoring won’t be a good fit for it, and neither will drugs that treat rare diseases. But other drugs with high volume and favorable side effect profiles will be a great fit. Think: is this a drug that you can see featured on Hims & Hers?
I think pharmaceutical companies are sick of getting taken advantage of by PBMs. PBMs have become increasingly greedy with their demands for financial kickbacks (ahem, “rebates”) from pharmaceutical companies. Even though PBMs have historically been seen as a necessary evil because insurance companies contract out (… to their own subsidiaries lol) what’s covered and what’s not, health insurance itself has become so expensive that people are opting to take the risk and go uninsured. From a patient perspective, the current pharmacy experience itself could not be worse—and honestly, it is downright inhumane at times. I think patients will happily choose to purchase directly from pharma in order to avoid the 20-minute line at CVS to talk to an iPad that can’t find your prescription.
[NK note: There’s a lot of conversation about direct-to-consumer pharma, Eli Lilly has this set up for a few different drugs on LillyDirect. Right now most of this just looks like a marketing funnel from Lilly to existing telemedicine pharmacies probably with some negotiated rates for the drug in the backend.
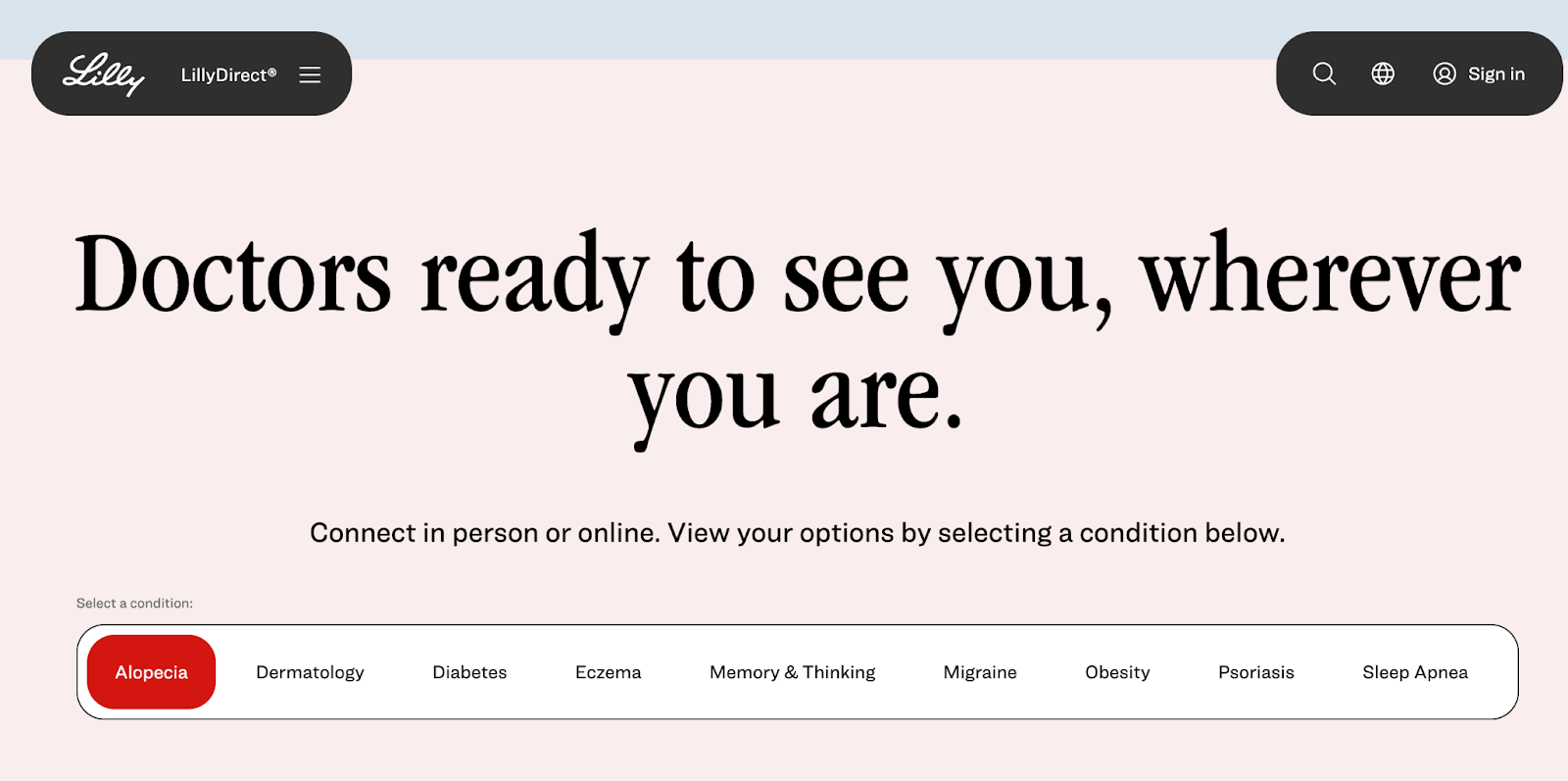
One of the more interesting podcasts of last year was the Eli Lilly CEO talking with Stripe founders. There’s an IRA double entendre to be made here but y’all aren’t advanced enough for that.
There’s a more interesting future he paints around whether direct-to-consumer could work for something like a one time gene therapy (e.g. PCKS9 edit in your liver), which provides a massive amount of value for a patient but not for a payer. Would a person pay a monthly fee for as long as that drug is working after that?
I agree that the d2c model will likely start with these drugs that already have massive pent up consumer demand, but it’ll be interesting to see how it further evolves.]
Happy new year
Wishing you all a happy new year!l It’s going to be a fun one.
We have a lot of really awesome stuff planned for this year. If you want to chat about working together on stuff, get in touch. Most of our content is sold out, and our inventory for events is going to go live starting next week.
Thinkboi out,
Nikhil aka. “I slept at 10 PM on New Years, just in case you were wondering”
P.S. Uhhhh we’re hosting a happy hour at JPMorgan next week but it’s gotten too big and now I need someone to help sponsor. If that’s you hit me up lol.
Twitter: @nikillinit
IG: @outofpockethealth
Other posts: outofpocket.health/posts
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







