Could Insurance Eligibility Checks Be Better?
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
TL;DR
Why’s it so hard for doctor’s offices to figure out if insurance is going to cover my visit? We’ll talk about why the process of an “eligibility check” is difficult.
Nirvana is a company that’s trying to make these eligibility checks easier and more accurate. We go through Nirvana’s product and some ways they’re working around existing data standards like X12, but we’ll also talk about whether this is a big enough pain point that they can break the curse of point solutions and force payers to play nice.
You can get a few credits to try your own eligibility checks for free if you say OOP sent you!
—
This is a sponsored post - you can read more about my rules/thoughts on sponsored posts here. If you’re interested in having a sponsored post done, let us know here.
Company Name - Nirvana
When Buddha sat below the Bodhi tree, it is said that it took him seven weeks to achieve Nirvana. After that he was without suffering or desire, and achieved a state of enlightenment.
Anyway this Nirvana is the complete opposite of that. It does eligibility checks - total pain and suffering- with the goal of figuring out what services are covered.

They also very explicitly told me it’s not Nirvana HEALTH. They are tired of the rest of you attaching “health” to semi-spiritual words, it’s not cool.
What’s the Pain Point Being Solved?
We have a very simple healthcare system. Depending on the permutation of your income, military status, age, state, and employment you will get thrown into a different type of coverage with entirely different rules. Even more fun, that coverage updates every year!
This poses many issues: it’s hard to figure out what you’re covered for, it’s hard for the doctors office to know if they’re going to get paid, and the process will suck all of the serotonin out of your brain stem.
When your doctor takes your insurance card for the 5th time, they partially do it to see your breaking point. But they’re also trying to figure out what the insurance company is going to cover, called an eligibility check. This will tell you:
1) whether your doctor is in-network
2) whether you are covered for that visit
3) how much that visit will actually cost
This sounds simple! “What could possibly go wrong?” said the main character, before the start of the horror movie.
Unfortunately, eligibility checks are a nightmare for many reasons:
First, a provider traditionally would send a request to a clearinghouse to figure this information out (called a 270/271 response). However, the data standard X12 that underpins this request is notoriously outdated. It can’t encode a lot of the information you might want and the outputs are extremely janky.
Second, the data is frequently not available in a basic eligibility check and it requires calling a payer to figure out what the contract says. Even then, getting the right answer is based on whether you’re talking to someone competent at the other end and whether the payer actually has accurate data about their contract with the provider.
Finally, the rules for payers are extremely complex and constantly changing.
- A patient might be eligible for Medicaid on their first visit but then their income increases and they’re no longer eligible by the third visit.
- A health insurance carrier might have their mental health network carved out, so you actually submit mental health claims to a different company.
- If you have a Blue Cross plan in a different state but get out-of-network care, you get billed at the rate of the local Blues plan.
And all of these rules also change constantly. The way that most practices handle this is by having a high-agency biller named Brenda or Marv who’s been with the practice for 20 years, seen every plan imaginable, and somehow stores all these phantom rules in their head.

But even then, eligibility checks still fail frequently. If a claim gets denied, the most likely reason is due to an issue with eligibility (20%+). If the eligibility check is wrong, it’s a huge pain for everyone downstream and causes a lot of frustration.
- The patient can’t tell which doctors they can see or not.
- The practices send a bill to insurance only to find out it’s been denied because the eligibility check was incorrect. Now they have to spend their time arguing with the insurance company.
- The patient was told they’re eligible when they weren’t, and now the provider is sending them a bill for whatever the insurance won’t cover.
- The patient can’t pay the provider, and now the practice has to write off the revenue.

What Does Nirvana Do? What Pain Point Do They Solve?
Nirvana focuses very specifically on solving the eligibility check, which they can do in a few seconds. It’s one step, but it leads to a lot of downstream billing issues if it’s wrong, so it’s very important.
You need as little as the patient’s name, date of birth, and zip code (for most patients, you don’t even need their specific insurance info). This can be embedded into a flow that already exists like the patient booking flow or in a standalone portal (e.g. the front desk staff checking your insurance info when you’re at the appointment). This can be done real-time via API or Nirvana’s platform (called OneVerify) one at a time or in regular batches.

Nirvana spits back the insurance details, in a JSON or single policy view in portal, including corrections they made based on things the Nirvana ML model identifies as incorrect (misspellings, incorrect payer, member demographic mismatches etc.).
This view shows the insurance information, whether or not the CPT code is covered, if there are other third party administrators or weird policies. It’ll also show how much the patient will owe based on the remaining amount of their deductible, coinsurance, co-pay, out-of-pocket max etc. I should hire someone named Max.
At an aggregate view, the dashboard will tell you how many checks had an identified denial risk or other alerts, what you might need to do to mitigate it, etc. Nirvana claims a 94% accuracy rate on what the patient owes on checks that they run.

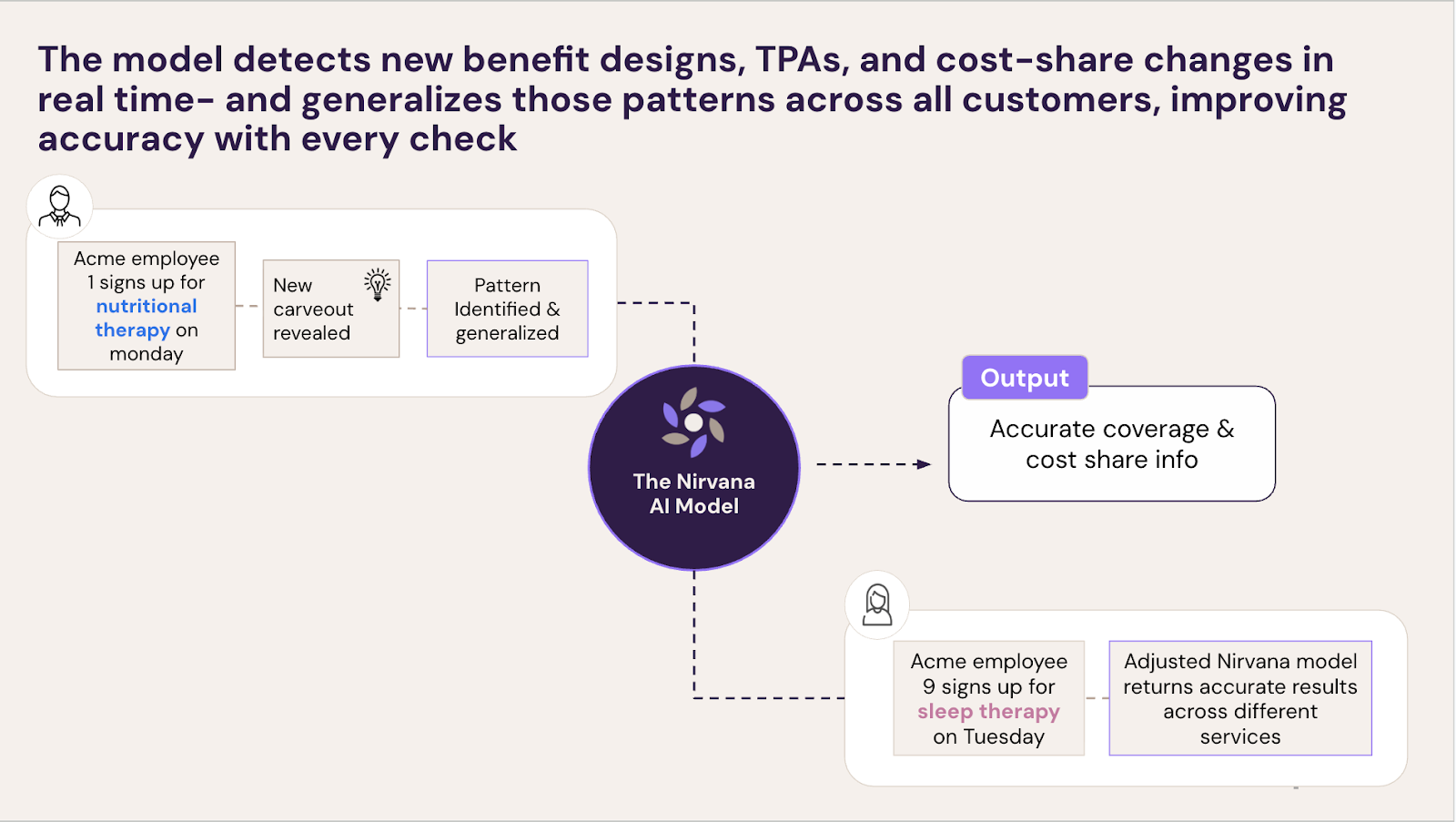
Under the hood, a few things are happening to get this information.
- They’re pulling data across the various clearinghouses to get the information they can about eligibility and benefits. But this data has holes in it or might be wrong.
- They pull in other datasets like claim remittance data and other proprietary data labels to triangulate information about benefit details, previous claims paid, whether they were paid, who paid it, etc.
- Every verification check is de-identified and used to train machine learning models and inform programmatic rules to improve accuracy performance across all patients.
- They use phone automation through the payer phone trees + billers on staff to annotate and check the responses that come back from payers.
For the people that know this problem intimately (which means it’s probably the only thing you know intimately), they’ve also built a specific product to handle this for Medicaid. In Medicaid, this area is particularly complicated because each state has different arrangements with the private health insurance carriers they work on what they cover, what the state covers, when a member is eligible for Medicaid, etc. On top of that, many Medicaid members don’t know their full payer information, so you have to figure out WHICH Medicaid plan they’re on by verifying with each plan!
What’s The Business Model And Who’s The End User?
Nirvana offers two pricing models: a pay-as-you-go option where customers pay for each eligibility check they run, or a committed-volume option with no per-check fees. The more you commit to buying upfront, the lower the price per check.
Their end users are typically billing, front office coordinators/intake staff, revenue cycle teams, or product teams managing patient sign up / intake flows at healthcare provider organizations.
Their sweet spot is providers that have a lot of visits where there’s a significant amount the patient will need to pay and there’s some level of insurance complexity in trying to figure out if there are denials.
They started in mental/behavioral health where the rules and carveouts are particularly complex and patients actually shop for a doctor based on whether they’re in-network or not. They’ve now been expanding into weight management, urgent care, imaging, sleep therapy, and gastroenterology practices.
Job Openings
You can find all of their open roles here, but some roles include:
- Forward Deployment
- Hybrid (New York City, NY)
- Machine Learning Engineer
- Hybrid (New York City, NY)
- Manager, Strategic Finance
- Hybrid (New York City, NY)
- Senior Backend Engineer (Integrations)
- Hybrid (New York City, NY)
[We’re so f***ing back, hiring engineers edition.]
Out-Of-Pocket Take
There are a few things I like about Nirvana.
Benefits complexity is going to increase - The general trend in health insurance right now is that the rules of coverage are getting more and more complex over time. Every new expensive service has new rules, every employer changes what they want to cover and carve out, and the number of medicare advantage plans have skyrocketed (each of which covers things differently).
When things were simple, a relatively adept coder could keep up with the relatively low permutation of plans and services that came into the office. But now the number of rules are far exceeding what billers today can manage.
In fact on the r/codingandbilling subreddit a lot of the conversation is about noticing trends in denials, how to navigate these rules, etc. Yes, I’m on the coding and billing subreddit. Don't snitch.
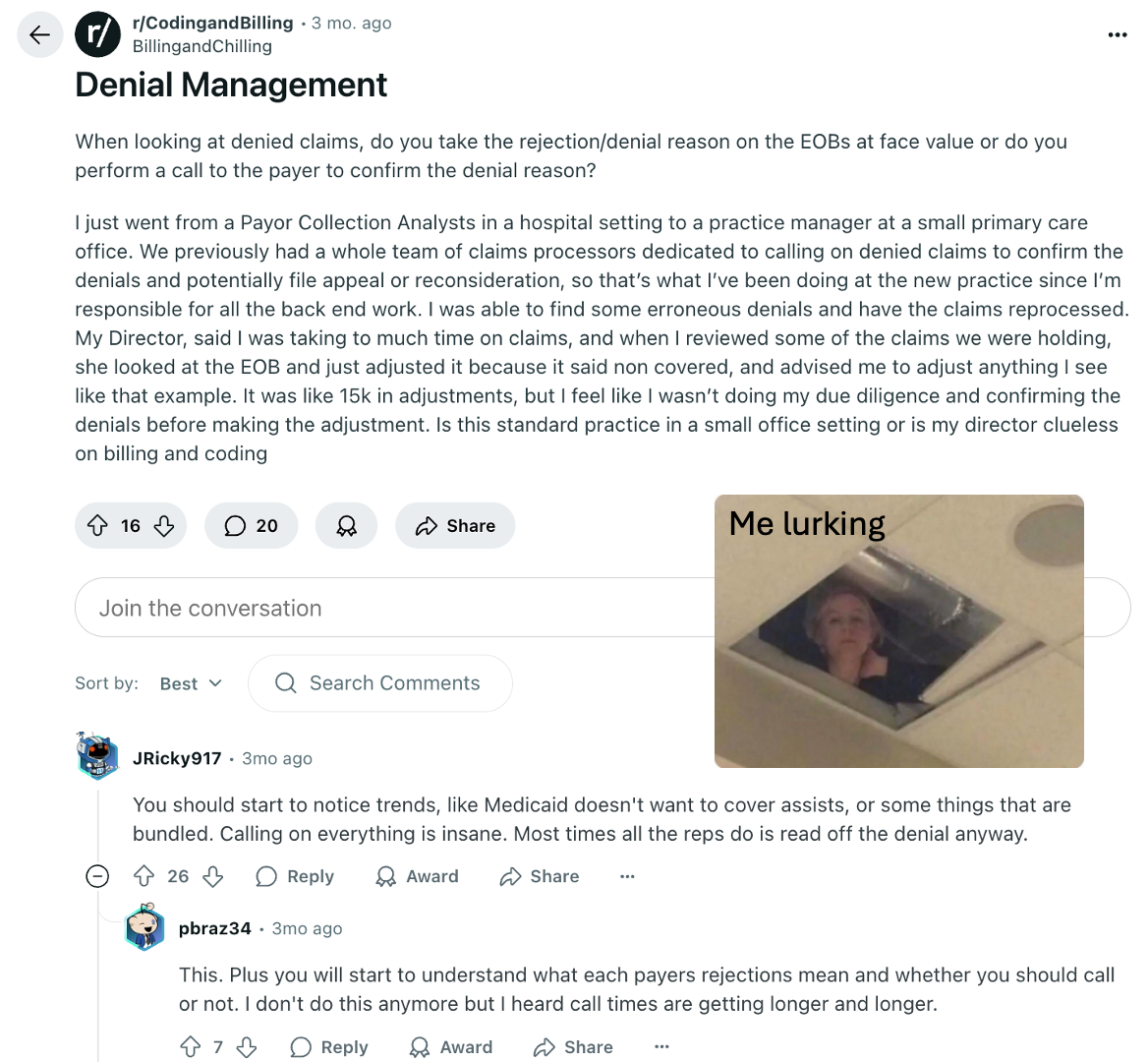
Even if someone starts noticing billing and denial trends, what do you do when that biller leaves? Nirvana’s bet is that instead of “noticing trends”, that AI can notice those patterns for you instead. Hopefully that can help practices and billers stay on top of these complex rule changes.
One, singular focus - The two most offensive things you could call a company are “lifestyle business” and “point solution”. You might as well just punch the founder in the face at that point.
I respect Nirvana’s focus on execution to do this one problem well and embrace the point solution moniker. There aren’t many areas in healthcare where the difference between being 80% good and 84% is a significant jump, but eligibility might actually be one of those areas. A lot of dollars are at stake based on this one step, so I do think it’s an area where being really focused on solving the problem can make sense.
The key though is they gotta execute.
They’re working around legacy standards - People in healthcare love to complain about the data standards used. “They’re too rigid, it’s outdated, everyone implements it differently.” - a crybaby
This is all true, but there’s a new wave of companies now that’re building around the data standards they previously complained about. A big part of this is that these new AI tools can make sense of edge cases and understand intent without needing to be beholden to a specific data standard.
Eligibility checks are a good example. Virtually everything that happens in this transaction- turning the X12 blob into JSON, parsing the documents in the explanation of benefits patients get to figure out coverage, extracting the right pieces of information from the electronic remittance advice that payers send back about coverage- are pieces of text flowing through. On top of that, you can use AI phone calls to verify information and get even more relevant information.
–
As with any company, Nirvana might face obstacles. Here’s what I see:
Point solution vs. platform? - Even though I just said that being a point solution might make sense here, I also have no spine in my opinions. It’s still going to be very hard to succeed as a point solution.
The open question is how hard is it for the platforms like EHRs or practice management systems to get to a 94% accurate eligibility check without needing to maniacally focus on it? Or for the clearinghouses to build a better product here themselves? Or if practices are fine with 80% accuracy?
This is the existential question that is making every AI startup founder religious, praying to Buddha.
Will payers play nice? - A lot of doing eligibility checks is an expectation that when you ping the payers to clarify some of the rules on coverage, that they will explain it to you. However, anyone that has called into a payer to clarify this can tell you that it’s basically a flip of the coin on whether they can answer. A big part of it is payers not having their own affairs in order. Things like knowing what’s in the contracts, keeping their directories up to date, and call centers that somehow gaslight you into thinking this is somehow your fault.
The reality is that the payers have not really had the incentive to fix this problem. Nirvana’s argument is that now payers have to staff up their admin and call centers to handle incoming questions about eligibility, and they can help them reduce that. Let’s see if it’s true! Because keeping the rules consistent between eligibility and actually being covered means payers actually being able to answer that question.
Expanding a customer base is hard - Nirvana has focused on mental/behavioral health, a space with lots of its own strange rules. But as they move to bigger customers and more traditional parts of healthcare, they’ll run into more friction:
- New sets of rules for different specialties with their own issues. Will their accuracy numbers hold as they expand into more complex areas?
- Different ROI arguments they need to make. Cost and coverage is a big consideration when it comes to mental health, but is it as big of a factor in decision making when it comes to imaging?
- Skepticism to automation and new processes from legacy billing teams that have done things for a long time and don’t want to switch to a new workflow. Can you teach an old biller new tricks?
But in order to become a big company, Nirvana is going to have to move into these new areas.
Conclusion and Parting Thoughts
There are lots of issues with US healthcare. But I think one of the most recurring frustrations that plague the bulk of the population is that they can’t answer two simple questions about a given visit.
- Am I covered?
- What is this going to cost?
We shouldn’t live in fear of what our bill is going to be, getting jumpscared by the mail 8 months after a visit. Figuring out eligibility is the linchpin of answering these questions, so if Nirvana can solve that (or at least push everyone else to solve it), then I’m rooting for them.
Thinkboi out,
Nikhil aka “what idiot called it ‘dating’ instead of eligibility check?”
Twitter: @nikillinit
IG: @outofpockethealth
Other posts: outofpocket.health/posts
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







