Personalized Health Insurance and the Payer Stack
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
Let me run you through a recent train of thought I’ve been having about what personalized health insurance products might look like. Follow me on this journey.
Medicare Advantage: An Early Indicator
I’m generally a fan of Medicare Advantage (MA). For the uninitiated, this is when the government contracts with private insurers to manage the health of Medicare enrollees. In an extremely simplified version, these carriers get paid a flat fee which is some base amount that gets multiplied by how sick the patient is.
But Medicare Advantage has several other quirks to it that are important to note:
- People looking for Medicare Advantage plans actually shop around vs. having to rely on an employer to choose options for them.
- Churn is pretty low in this population and the amount you get paid per enrollee is quite high. A lot of money goes into acquiring beneficiaries and you can make the economics of a plan work with a relatively small number of beneficiaries compared to other health insurance segments.
- Your payment gets adjusted for the risk of the population you take on, so there isn’t an issue with making a plan that might attract a particularly risky population.
- The rates for different healthcare services are fixed in Medicare vs. commercial insurance where plans have different prices all over the place. This means that the main lever MA plans have to keep costs low is to REDUCE using healthcare services at all, especially high cost things like a preventable hospital admission (e.g. a member falling and breaking their hip). This means it’s very worth it to invest heavily in upstream services like primary care and home visits for at-risk people.

- MA gets some flexibility in terms of what can be covered as a medical expense. This includes things like meals, transport, vision, etc.
Because of this, there’s an interesting trend where MA plans are trying to attract more and more niche populations. This includes wrapping around different “front door of healthcare” options (e.g. pharmacists, integrative medicine physicians, etc.), reducing co-pays for different services (e.g. acupuncturists, herbal supplements), putting an emphasis on the languages physicians in their network speak, and more.
There are a few key advantages by creating more targeted insurance products. For one it becomes easier to target your marketing and potentially get word of mouth effects as beneficiaries refer others in their community who might have similar needs. Also if the goal is to keep consistent tabs on your beneficiaries so they don’t end up in the hospital, you want to make sure they regularly go to whatever their version of primary care is.
Clever Care for example is an MA plan that targets members who want more eastern medicine options. Humana was hiring a product manager to build plans targeting Korean and Chinese beneficiaries.

Here is a bit about Alignment Healthcare, who’s planning to create several different demographic targeted plans under the larger umbrella.
“Alignment Healthcare personalizes these plans by adding benefits that target social determinants of health, like a pre-paid debit card some HMO enrollees can use to buy health and grocery products or to install a home security system. In California, the company created a benefit package called Harmony for Asian-American policyholders. Beginning with that population was natural, Kao said, because he was born in Taiwan and has a personal interest in the wellbeing of Asian-Americans.
Going forward, [Alignment Health CEO John Kao] said the insurtech plans to unveil more health plans targeted at groups, like Hispanic and Black enrollees.”
Beyond demographics, Medicare Advantage also has a subset of available plans called Chronic Special Needs Plans (C-SNPs). These are plans that design their network, prescription tiers, cost-sharing (e.g. $0 premiums for certain things), and supplemental benefits to target Medicare beneficiaries that have one of 15 designated conditions. For many people, most of their care revolves around the management of a specific condition, and these insurance products cater to that. After a few years of contraction, C-SNPs seem to be growing in the last few years (you can see some examples from Anthem here).

In general, I like this trend of targeted insurance products. I think it actually allows buyers to find plans based what they’ll actually use regularly aka. primary care-esque things and lifestyle benefits. I expect more personalized insurance products to take off in MA.
Personalized Insurance In Other Markets?
This train of thought now takes me to the next point, which is my belief that more insurance segments will eventually start looking like Medicare Advantage and employment/insurance coverage will have a way weaker tie in the near future.

Specifically my hope is that in the individual exchanges you’ll eventually see:
- Individuals having the same tax-benefitted dollars that employers currently have
- People actually shopping around (preferably on a non-state run exchange website that has the functionality of ass)
- More flexibility around what can be covered
- Less churn
- Better risk-sharing/risk-adjustment that accounts for how sick a plan’s members are (the individual exchanges do have this, but historically the government has not been great about stabilizing the risk of this pool + it’s a “zero sum” risk pool between the plans)
Yes, these are high hopes. Employers are really deep in it when it comes to health insurance. But there are some promising signs. The courts ruled “ACA good”. The boy JB has increased subsidies to help people afford their premiums on the exchanges. There were talks of a public insurance option in different states like Washington, Colorado, and Nevada. ICHRAs...exist (I’m hoping they see more adoption because they let employers give their employees their tax-benefitted dollars to buy plans on the exchange). More companies going remote means less geographic density in any one place so they might find it easier to let employees buy on their local exchange instead of trying to fit everyone into a national plan.
Plus enrollment seems to be trending back up after a few lulled years + the margins per member also seem to be going up. So plans like Aetna and United that left the exchanges are starting to look back at it (feat. A Boogie Wit Da Hoodie).

Beyond that, I think employees are pretty tired of the options they have available through their employer. These are plans designed to be “good enough for the bulk of your employees” but not great for anyone. Combined with a tight labor market, maybe employers are more open to letting their employees find plans that work for them.
I’m optimistic about the individual exchange and expect it to be one of the faster growing markets. I’m also hoping that it means we’ll see more of these personalized plans popping up as a result as well if the shopping behavior tracks at all similarly to Medicare Advantage. This isn’t a totally novel idea - Cigna has a diabetes insurance plan for individuals, and CCHP is an integrated delivery system combining different health insurance products with providers at the Chinese Hospital, Chinese Community Health Resource Center (CCHRC), and Jade Health Care Medical Group.
My hope is we’ll see more of these targeted plans.
Who is building the new payer stack?
There has been an explosion of personalized primary care companies. There are primary care/care team companies focusing on demographics (e.g. Spora), sexual orientation (e.g. Folx), age (e.g. Iora), conditions (e.g. Thirty Madison) and more.
One of the enabling reasons for this is that an entire segment of infrastructure companies have spun up to make the formation of new care delivery models easier. Don’t wanna do your own pharmacy fulfillment? There’s an API for that. Wanna make credentialing easier? There’s also an API for that. Wanna dismantle the social construct of reality? There’s an API for that too. Julie Yoo of Andreessen Horowitz outlined a lot of these companies in this talk + graphic.

I think having more personalized insurance products is the natural extension of this trend. It’s not just having primary care that’s more targeted to you, but that you’ll be covered for the follow-up services and therapies that are recommended to you. Hopefully the rise of the individual exchange makes it more feasible to build these personalized insurance products.
In which case, what is the infrastructure stack that would make it easier to build a new health insurance carrier on top of? Many of the companies in the stack are building products for providers that on the flipside also make it easier for new health insurance carriers to plug into as well. Some companies like HealthEdge are already doing this and seeing new health insurance carriers built on top (like Friday Health Plans).
Rattling off some random functionalities that could help build the new payer stack:
- Provider directories - Insurers have to keep their directory of in-network providers up-to-date or get hit with nasty fines. Beyond that, if you wanted to find physicians in-network that had certain characteristics (e.g. spoke different languages) you’d probably want that in your directory too. Companies like Ribbon are tackling this, and they’ve also launched a product that lets you see if a physician sees other patients like you (demographically, condition-wise, fears/dreams?, etc.).
- Provider contracting + network optimization- Building out a provider network is a huge pain in the ass. You have to negotiate prices, you pay consultants to help you figure out market dynamics, you wrangle together excel docs, and then go back-and-forth through emails. You can rent network rates through companies like Magnacare, but they’re expensive and don’t give any flexibility. I’m an investor in a company called Turquoise Health. Turquoise Health is releasing a new Clear Contracting product that makes it way easier to set up and adjudicate negotiated rates and you can eventually even build your own bundles, etc.

- Claims processing - There’s an entire process that happens in the back end when a provider files a claim with an insurer. It involves checking if the provider is in-network, how much of your deductible you’ve hit, making sure there aren’t errors/duplicates in the claim, what the negotiated rate is, etc. Historically this was a lot of paper and faxes flying around everywhere so the processes became extremely labor intensive. But the claim is a key pillar of any insurance business - it dictates how money should flow which leads to every single follow-up process with the patient or provider. It’s so critical that Oscar built their own claims processor in-house, and now plans to let others build on top of it.
- Pharmacy Benefits - Most payers rely on Pharmacy Benefit Managers (PBMs) to deal with pharmacy claims, negotiate with drug manufacturers, and figure out what medications should be covered in a patient’s plan and the cost they’ll pay. While unfortunately this is a business that favors massive players with negotiating power, maybe some of the new tech-enabled players like SmithRx can do some interesting things with formulary design.
- Finding Good Physicians - Every health plan wants to have the “best” physicians, but the reality is that there is no universally agreed on metrics to identify “best” and each patient will care about different things. You might care about surgery outcomes. I care about whether they call me “champ”. Companies that do quality scoring of physicians like Garner Health can help identify high performance physicians in an area that might matter more for the target demographic you’re selling the plan to (e.g. if they’re more likely to have a certain procedure, then having that physician in-network is more important).
- Utilization Review - When a health insurance carrier is on the hook for a particularly large bill it will likely go into something called utilization review. This usually involves some clinical person on the insurance side (e.g. a nurse) making sure that everything the patient received was following the protocols in their plan. You can outsource this to companies like evicore today. I could see someone like Wheel or another company turning this into largely gig work that programmatically checks the rules of a plan, has someone clinical make sure the patient’s treatment wasn’t out of line from the norm, and check if the patient/provider followed the plan's rules for coverage.
- EMR <> Payer Data Exchange - Having an EMR feed between the physician and the payer can make it easier to deal with things like prior authorizations, billing + coding, etc. Companies like Canvas are interesting to me because they have a Software Developer Kit that the payer can use to inject rules into the EMR. This way, the physician is given reminders about things to note or stuff to do with the patient to make sure things are covered and there won’t be issues weeks later when the payer deals with the bill. It feels like new payers that want to enter into different kinds of value-based care arrangements would like something like this since they can give reminders to the physician at the point of care instead of needing to retroactively deal with it. If not a new EMR, it could also be the many companies that are riding the interoperability rules which both payers and providers need to comply with (and generally stop crying about it). Payers and providers need to make it easy to pipe patient data out through standardized APIs, and companies like Innovaccer, 1up Health, etc. are trying to make it easier to be compliant and share data between the two.
One of the real benefits here I think will be using EMRs as a conduit to highlight personalized treatment pathways and updated evidence-based guidelines for specific groups. This would require providing coverage and nudges for certain types of screening for certain subgroups. For example, the American Heart Association has identified several ethnic subgroups as particularly at-risk for cardiovascular issues that should probably have screening covered earlier. Or for people in a sickle cell crisis (a disease that predominantly affects Black patients) it might make sense to nudge and cover transportation to a specialized infusion center which has better outcomes than going to the ED. Coverage for follow-up services specific to a group needs to be reflected in plan design.
- Subnetwork contracting + credentialing - New payers might want to bring in new forms of care that have traditionally had difficulty getting reimbursement (doulas, naturopathic physicians, therapists, my weed dealer, etc.). Companies like Headway have made this easier to get therapy that’s in-network by dealing with the back-office processes that a therapist normally doesn’t want to deal with to be in-network. Maybe we’ll see other companies like this for other parts of the care team so new insurers can easily get them reimbursed and in-network.
There are so many more I’m probably missing. Sending patients materials, their insurance card, or explanation of benefits? Lob has a direct mail API. Wanna add an HSA? Throw in Lively or First Dollar. You can easily embed acute telemedicine services into any payer app with the million telemedicine companies like Teladoc, DrOnDemand, etc.
I’m sure there will be call centers that are easy for payers to plug into that triage the incoming call and escalate it to the correct person depending on how much clinical knowledge is necessary to answer member questions. Who’s building outsourced actuaries to help analyze insurers understand their member population risk in real-time (maybe Cerebrae)? Idk I’m riffing at this point.

I’m sure there are some grizzled healthcare vets who have lost any spark of joy in their eyes that will say “outsourcing, you invented outsourcing”. They’ll point me to some old school company with 50 consultants and one IT person, and claim it’s the same.
Third-Party Administrators (TPA) are companies that usually handle a lot of the above services. However most of them are designed to target the employer insurance market and suck to work with. This is especially true if you’re a small customer or want to build some sort of automated process that requires data passing between you and the TPA. Some of the newer TPAs that currently target the employer market like Flume Health might do this better + have a stack other payers can build on top of. But in general, it’s a very different business when you have two computers talking to each other vs. two people that have to schedule monthly check-ins to get anything done.

One of the benefits of having a new insurance stack is that it’ll be easier for new payers to keep their administrative costs low, which is important because individual exchange plans have to spend 80% of the premium dollars they collect on claims. The leftovers are usually slim pickings that go to admin and profit. This is also a reason why I think current health insurance carriers are reluctant to upgrade their infrastructure - because it’s usually a massive upfront cost which is hard to make work when you’re capped at 20% of your spend for admin stuff. The inability for incumbents to make massive infrastructure investments is an opportunity for new carriers that are building on top of a new stack from the beginning.
Parting thoughts
I know it’s a long shot to believe that we’ll see lots of new carriers on the exchanges. Oscar and Bright had to spend a bajillion dollars to get there with debatable success. Regulation makes it difficult to actually be flexible with plan design. If you attract a high-risk population you’ll go bankrupt. Member churn makes it difficult to invest in the health of patients. The market is still tiny. But it wouldn’t be any fun if we all agreed on trends right?

But my hope is that this plug-in infrastructure makes it easier to spin up plans and experiment with things like network design, covering different goods/services, and more. Today most people are pretty unhappy with what they get with their health insurance despite paying more every year. We should want more plans competing to give us more personalized options.
A few miscellaneous thoughts:
- One of the big open questions is the role of the insurance broker in these scenarios, who are trusted advisors for many folks choosing health insurance plans. Do these plans empower brokers with tools to help sell plans that are personalized? Can these plans disintermediate brokers by going to other community members delivering care (e.g. if an acupuncturist has a small handful of plans that fully cover their care, they’d be more likely to recommend their patients get that plan).
- I’m not even sure there are enough primary care, caregivers and other frontline options that are trained to be attuned to the care of specific demographics. This pool will have to widen if new payers want to scale nationally or want to nudge referrals to these options without having insanely long wait times.
- How many carriers will want to outsource these functions to the “insurance stack” companies vs. in-sourcing them? Everything outsourced is both a loss of control and loss of potential revenue to be captured (e.g. the PBM function). This could potentially force new insurers to churn off these stack companies eventually.
- When are we going to have creator driven insurance products? I’d probably buy OVO health insurance from Drake.
If you’re building a new targeted health plan or part of the stack that payers can build on top of let me know. I’d love to chat. We can confirm each other’s existing beliefs to further convince us we’re on the right track.
Thinkboi out,
Nikhil aka. “I really need to stop relying on bullet points to articulate disjointed thoughts”
Twitter: @nikillinit
Thanks to Sahir Jaggi, Frank Wu, Jeff Yuan and Anonymous for reading drafts of this post
---
{{sub-form}}
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
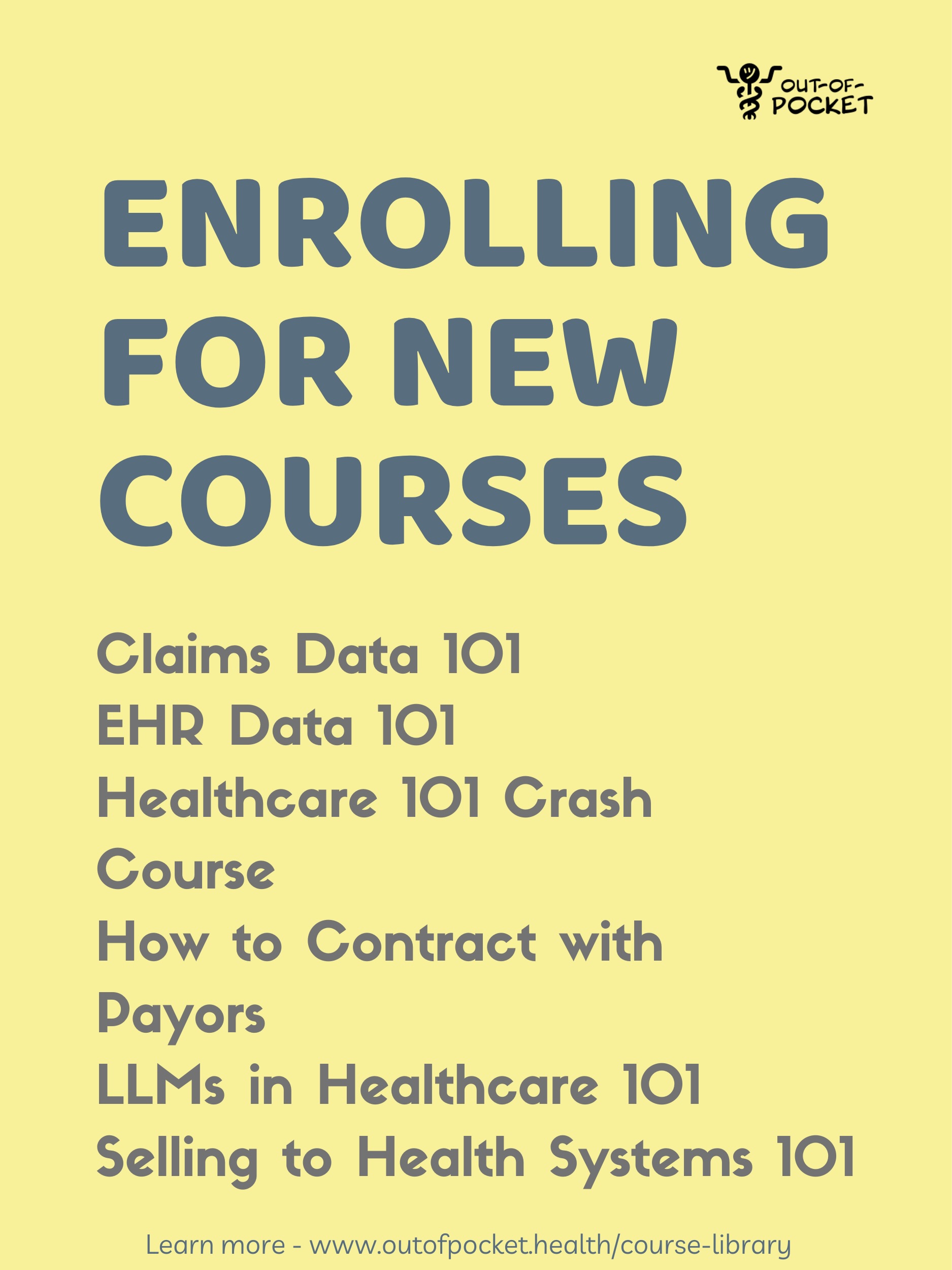
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.