Retail and community pharmacies are changing
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
After John gave me an excellent interview that explained how pharmacies work, I dove a bit deeper.
I’m interested to see how the role of retail/community pharmacies and pharmacists changes post COVID. A lot of trends that were already happening are now being exacerbated + new opportunities are opening.
For one, the COVID vaccine is probably going to be distributed in some capacity via pharmacies. Walgreens and CVS have both announced this. This is going to give pharmacies a window to get a lot of people in their stores and show off the health programs they have to offer.
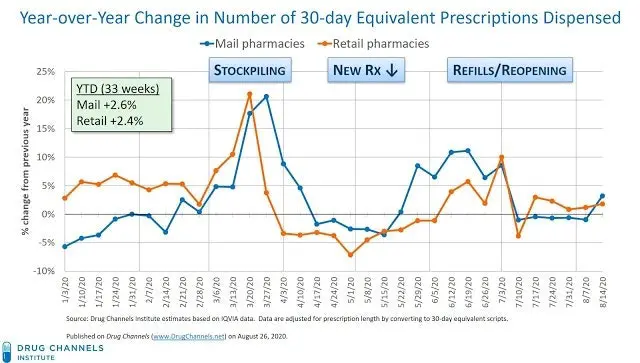
Second, I’m going to bet that enrolling in mail-order pharmacies becomes more common. Frankly, I’m surprised the data suggest that mail order hasn’t actually surged during the pandemic (other than the stockpiling phase). But I feel like Amazon’s recently announced push into mail-order pharmacy is going to spur more initiatives from every mail-order pharmacy player to convert more members to a mail-order pharmacy.
I could be wrong about mail-order finally taking off; but if it does then it’s bad news for retail pharmacies (unless they make a few changes which I’ll talk about below).
Third, the surge in cases (especially rural areas) and the need to distribute the vaccine quickly means that we’ll need as many clinical staff as possible to manage non-emergency patient care. We can use this opportunity to better use pharmacists/pharmacies as a part of delivering care, monitoring patients post-vaccine, and maintaining touch points with chronic disease patients. This is going to be especially true in rural areas.
All-in-all, to me this marks a definitive turning point where retail and community pharmacies need to shift away from the current model of maintaining brick & mortar stores for the sake of selling different types of goods and instead use their position within communities and with trained staff to become services businesses.
Some specific shifts I’m watching.
Pharmacies as micro-fulfillment centers
I was once talking to someone from Brazil who was in the US for grad school, and I asked them what was something that surprised them about the US. They jokingly answered “I don’t know the difference between your grocery stores and pharmacies.” And something something about how the US system of democracy relies on an electoral college proxy which re-weights individual votes and undermines the purpose of having a direct democracy but whatever that wasn’t the important part.
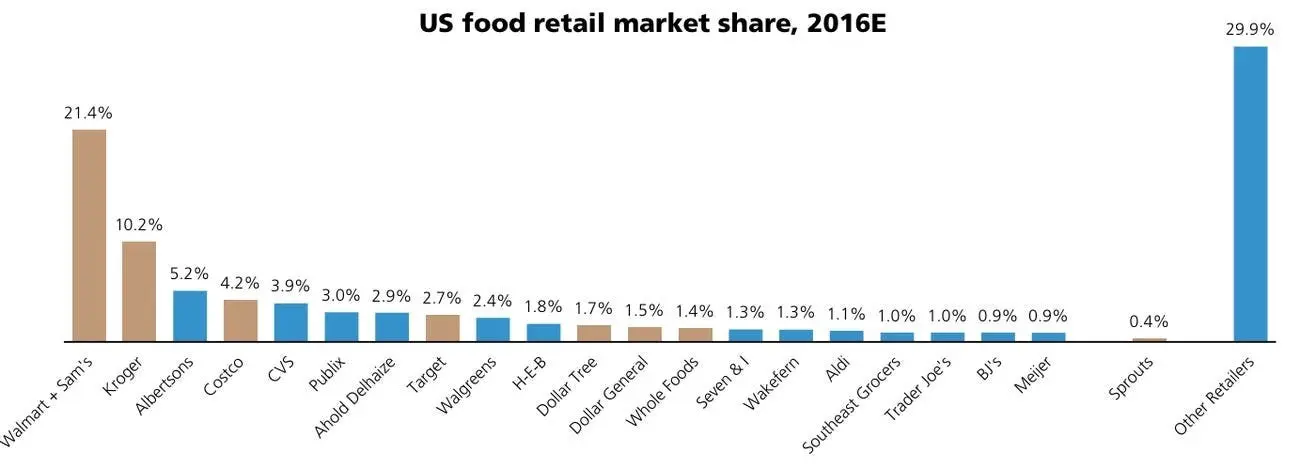
I recently went to Walgreens and thought to myself “huh, I guess it is kind of weird I can get Chateau Diana, milk & cookies, and topical ketoconazole in one place…” despite how fun of an evening that sounded. And the data shows that basically every single one of the top 10 grocery stores by market share is either a "grocery chain with a pharmacy” or a “pharmacy that also sells some groceries”.
Historically pharmacies have sold a host of different products to offset the costs of the more expensive real estate and drive foot traffic into the store. Fun fact - Walgreens actually grew as an enterprise because they differentiated their pharmacy with hot food and a “Walgreens special malted milkshake.” They even had a bakery! Eventually this morphed into more of the shelf-stable and frozen convenience food items you might see today.
But today things are changing. I think we’ll see pharmacies fracturing into different types of micro-fulfillment centers.
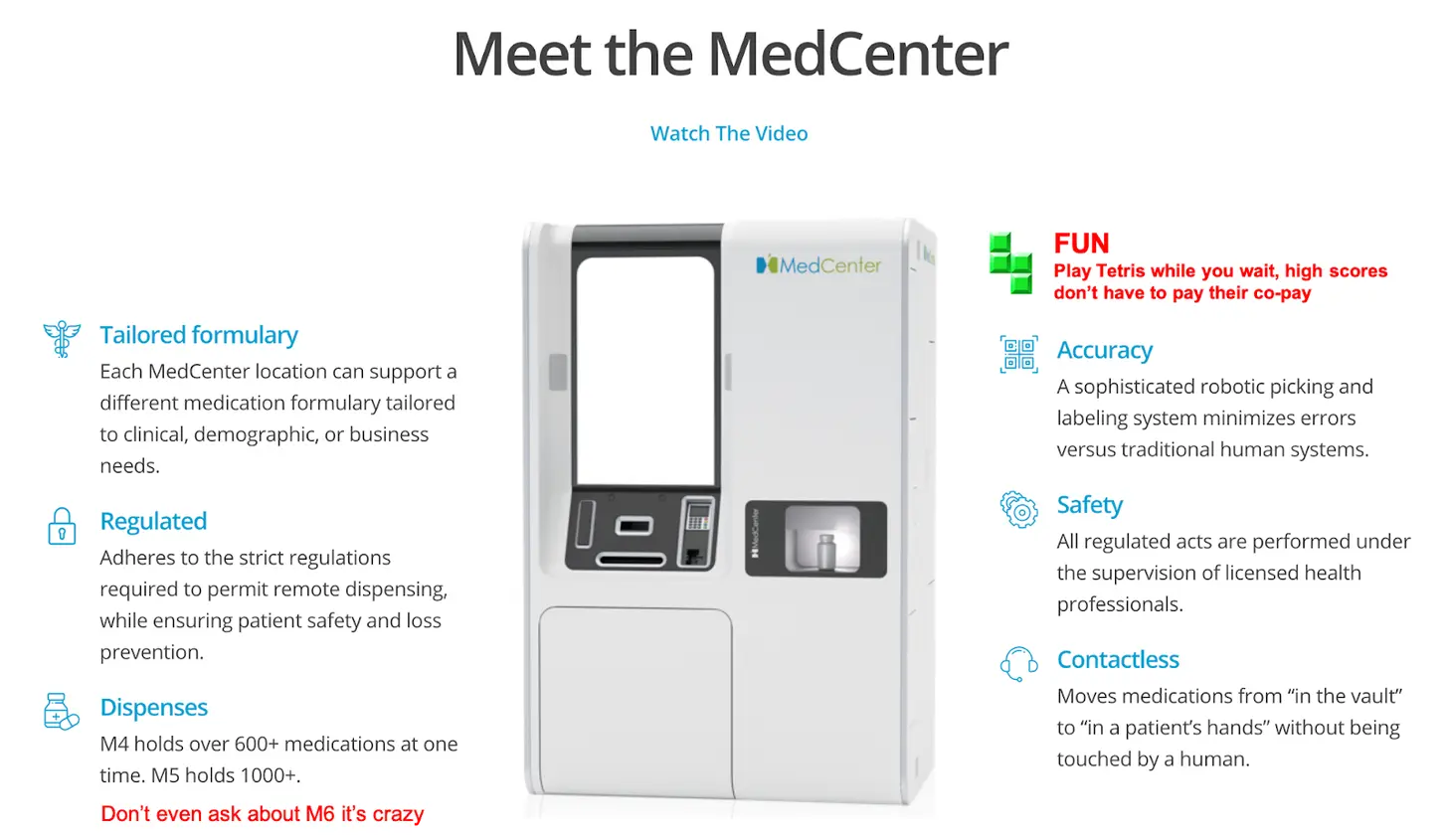
We’re already seeing a few versions of this. One is with pharmacy vending machines with tele-pharmacists like MedAvail that can dispense common medications.
Another is same-day delivery pharmacies like NowRx, Alto, and Capsule which have smaller physical footprints and cover a much larger geographical range than traditional brick-and-mortar pharmacies. Very curious how these companies can make the unit economics work but that’s probably a separate conversation.

Or eventually you’ll see all-in-one last mile delivery micro-fulfillment centers that bundle all same-day needs together (grocery, pharmacy prescriptions, etc.) through networks of micro-fulfillment warehouses. This seems to be where companies like Uber (moving into groceries and pharmacy), Amazon, and Walmart are slowly moving. Throw in some robots for last-mile delivery (which CVS has piloted) or drones (which has also been piloted) and you basically have removed the need for expensive real estate based pharmacies for any medication that doesn’t have any weird administration requirements like an infusion, etc.
With these micro-fulfillment centers, you’ll see one type of retail pharmacy that exclusively focuses on dispensing medications in the most cost-effective way. This leaves room for a second type, which focuses more on services.
Changing the role of the pharmacist
There are some contextual points to understand about pharmacies for the uninitiated (aka. me 48 hours before the publication of this post).
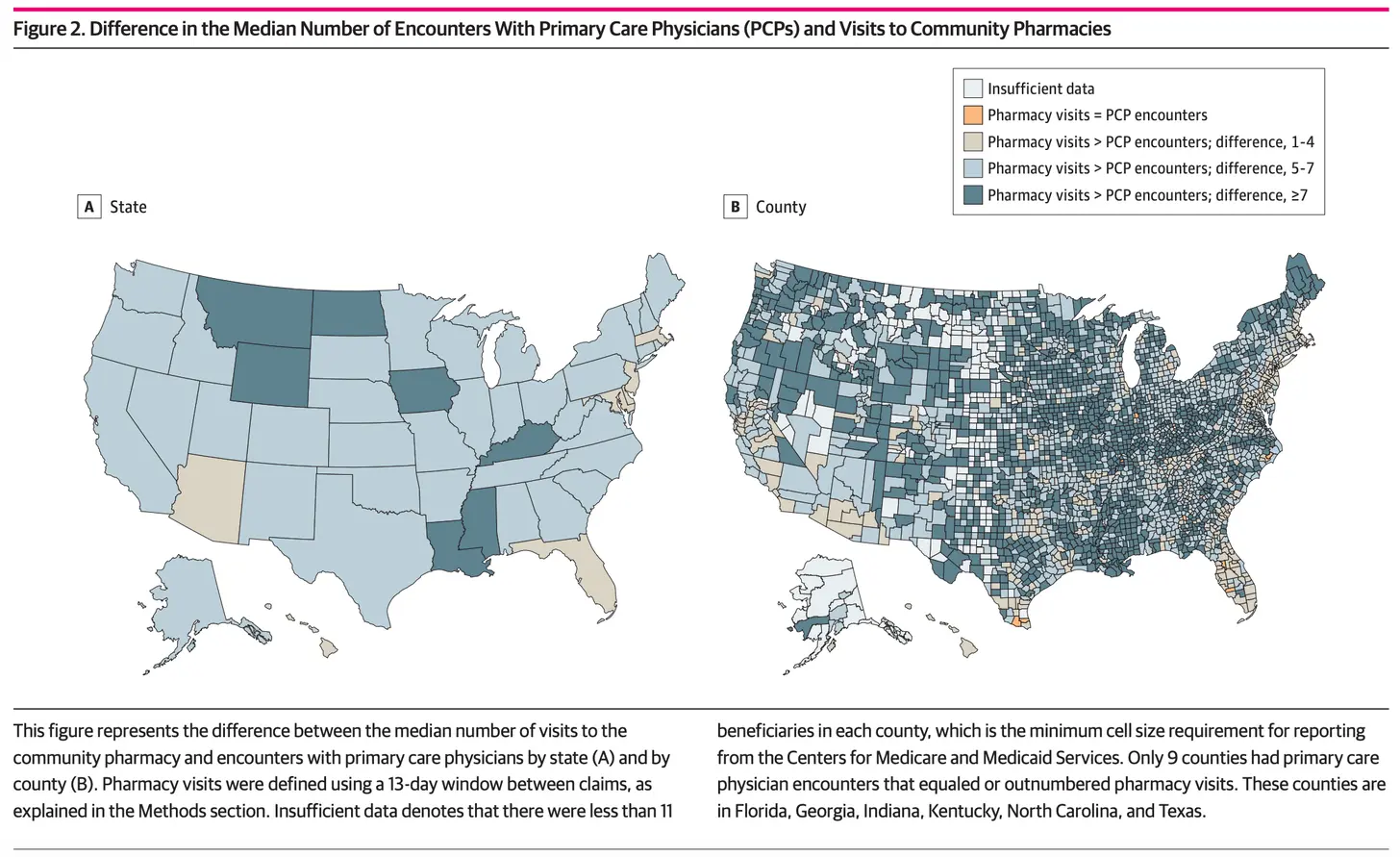
More than 90% of the population lives within 5 miles of a pharmacy. There are about 327K pharmacists in the US and 486K total primary care providers (internal medicine, family medicine, pediatrics, etc.). Medicare beneficiaries, who are more likely to be on a recurring medication, see the pharmacist twice as often as their primary care physician. Twice as often is the median; in more rural counties with primary care shortages, it can be more than 7x. This is for a host of reasons like physical accessibility of the stores, short wait times/no appointments needed to see a pharmacist, and it’s $free.99 to chat with them.
Pharmacists are an underutilized part of the clinical staff, and unlike primary care physicians there’s actually no shortage of pharmacists. Historically, their role has been focused on the dispensing of prescriptions. They’ve focused on things like: Is the prescription that’s coming in correct? Is it being filled and formulated correctly? Are there potential drug interactions that should be flagged? Does the patient understand the side effects?
Today’s pharmacist is trained way beyond dispensing tasks. Starting in 2004, pharmacists were required to have a doctorate degree (PharmD) to even get entry level roles so they get more clinical training than pharmacists of the past. Many also complete residencies to get more clinical experience and/or specialize (it looks like there are >5K residency spots per year).
We need to change the scope of work for pharmacists - partially because computers can now help do some of these tasks much more efficiently and because the reimbursement per prescription has been consistently decreasing. This has led to chain pharmacies pushing pharmacists to work crazy volumes, hit target metrics, and more while decreasing staffing levels.
Nearly everything is tracked and scrutinized: phone calls to patients, the time it takes to fill a prescription, the number of immunizations given, the number of customers signing up for 90-day supplies of medication, to name a few.
The fact that tasks are being tracked is not the problem, pharmacists say, as customers can benefit from services like reminders for flu shots and refills. The issue is that employees are heavily evaluated on hitting targets, they say, including in areas they cannot control.
…
Staff members were supposed to persuade 65 percent of patients picking up prescriptions to sign up for automatic refills, 55 percent to switch to 90-day supplies from 30-day, and 75 percent to have the pharmacy contact their doctor with a “proactive refill request” if a prescription was expiring or had no refills, the documents show. - New York Times
Certain rules and regulations that were initially designed to promote patient safety (e.g. pharmacists having to visually check every single script) are now working against their intentions. We need to shift more tasks pharmacists do (e.g. visual inspection, looking up data, dispensing, etc.) to software/machines, which might actually perform equally as well.
Instead, the role of pharmacists will likely need to shift to focus on the human facing side of things and areas that are more cognitive which pharmacists don’t have time to do today. This has included everything from counseling patients on their medications, interfacing with physicians on how medications fit into the care plan, diving deeper into drug-disease or drug-lifestyle interactions (which requires understanding more contextual data about a patient outside of just their medications), etc.
Medication Therapy Management was a first step in this direction and reimburses pharmacists for tasks that are outside just dispensing medication to provide other services like reviewing medications, creating action plans that combine lifestyle changes with medication changes, connecting patients to the right follow up care, etc. However from people I’ve talked to, the economics currently don’t work out - pharmacists don’t really get reimbursed enough to make it worthwhile despite it seeming to save costs in the long-run. Plus, unless pharmacists are explicitly integrated into the primary care team, the reports they send can end up just sitting in the PCPs fax machine.

There are some new experiments happening to expand the scope of pharmacists that I’m watching:
- In Florida, pharmacists can now diagnose and treat lower-risk non-chronic conditions like strep, flu, lice, etc. and certain outlined chronic conditions (with the expectation of expanding into others). They work in conjunction with a patient’s physician through something called a collaborative practice agreement which allows a physician to shift some of these activities to the pharmacist.
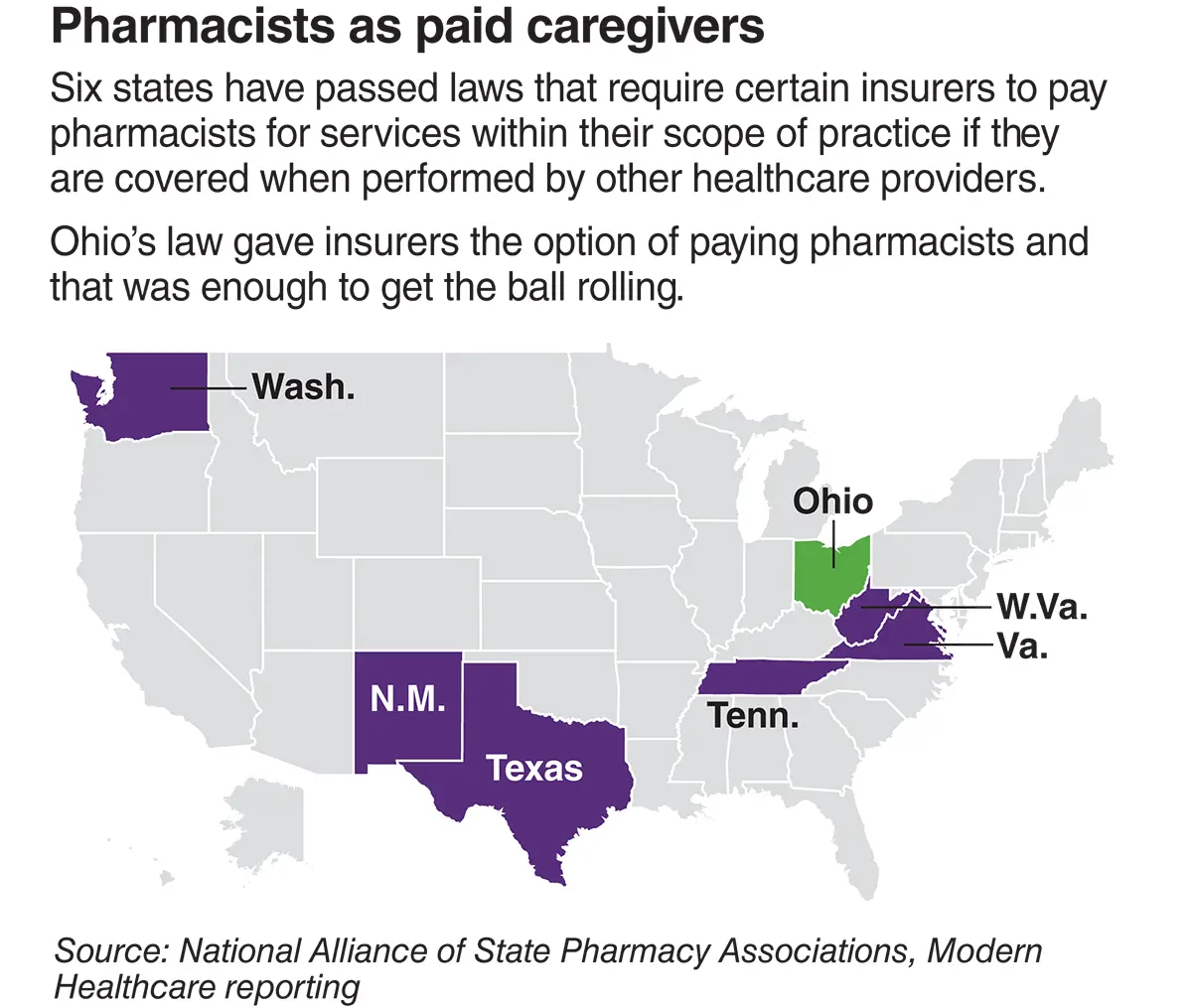
- In Ohio, Medicaid officially recognizes pharmacists as healthcare providers and allows Medicaid plans in the state to pay for certain pharmacist services under their medical benefit. This enables pharmacists to get that provider bread (though whether or not it’s enough to cover operating costs is still a question).
- Medicare-focused primary care startups + MA plans are looking to embed pharmacists into the general care team for patients as a lower cost form of labor that has more touch points with a patient. Troy Medicare recently raised $10M as a Medicare Advantage plan that wraps around independent pharmacies. VillageMD is now posting up in Walgreens to create a primary care + pharmacist integrated approach for patients with complex medication regimens. Walmart is bringing primary care to their stores and pharmacists are already positioned to provide assistance.
“We offer a wide range of clinical services, such as year-round immunizations in 49 states and Puerto Rico,” she said. “Our pharmacies, where allowed in the state, provide CLIA-waived screenings and, in select locations, rapid diagnostic testing. Our MTM/adherence program includes adherence outreach, gaps in therapy, targeted and comprehensive medication reviews, medication synchronization, refill reminders, and messaging.”
…
“Our pharmacists prescribe and counsel on Naloxone, and are engaged in a comprehensive opioid stewardship program. In specific locations, we offer prescriptive services, including hormonal contraceptive prescribing and treatment for minor ailments. We have a full service specialty pharmacy and also offer select specialty products in our retail locations.
…
Our pharmacists are well placed to coordinate care for patients with multiple providers and specialists to help ensure all the medication and services they receive are working together appropriately for the best outcomes for the patients. Collaborative practice agreements are in practice, where allowed in the state, for immunizations, rapid diagnostic testing, health screenings for public health, oral contraceptives, and naloxone dispensing and counseling.”
- Hospital-at-home models are poised to increase in popularity thanks to CMS giving their blessing. Deploying pharmacists for patients that have complex medication regimens that need to be monitored closely will likely be key to reaching cost savings.
- I’d like to see more exploration of embedding pharmacists into the community settings they’re already a part of. We’ve talked about pharmacists in barbershops. CVS seems to be building affordable housing in Orlando and expanding their screening programs there (which I assume will eventually include bringing pharmacists to housing developments with a large % of at-risk patients). Bring the pharmacist + screening tools to people instead of just getting people to come back to the pharmacy!
Even though pharmacists can do more and get paid for services now, this will be for naught if we can’t shift some of the dispensing focused tasks away from pharmacists, make the economics work, and get providers on board to (easily) bring pharmacists into their workflow.
Pharmacies as the online-offline handoff
We are currently in a boom of virtual chronic disease management companies. I can’t even enjoy breakfast in peace in the mornings because I’m just bombarded by PR firms whose lists I never signed up for sending me more press releases about their chronic disease management companies raising another $X million dollars. How are there so many of you???
*deep breath*
Anyway as I said in my Teladongo piece, I think one struggle that virtual chronic disease companies will have is connecting those patients to in-person care when necessary. I think pharmacies can play a role here with the in-person referral as needed. Pharmacists would determine whether the patient’s medication and lifestyle regimen needs to be adjusted, order labs/collect samples from a patient, guide patients through in-person screening, and relay that information back to the coach/physician/team at the chronic disease company. Thanks to improved software that can do things like scan for diabetic retinopathy, monitor diabetic foot ulcers, check for heart rhythm abnormalities, etc. we can actually distribute the expertise of specialists and just need a person to help walk a patient through the screening procedure.
Companies like higi seem like they’re directionally going this route by placing their measurement systems in in different pharmacies. They can capture basic measurements (blood pressure cuff, BMI, weight, and pulse) but honestly, these machines seem huge. So I assume/hope they start stocking them with more of these advanced screening tools for other chronic disease screens.

Community pharmacies could be a great, accessible way for virtual chronic care clinics to get their members the in-person care they need, especially with these new tools.
Pharmacies as a diagnostic and escalation hub
This one is a bit more of a stretch, but I think it would be interesting.
As a society, it seems like we're leaning more towards putting diagnostics- which have some % of false positive rates- in the hands of consumers. At population scale, that’s not insignificant.
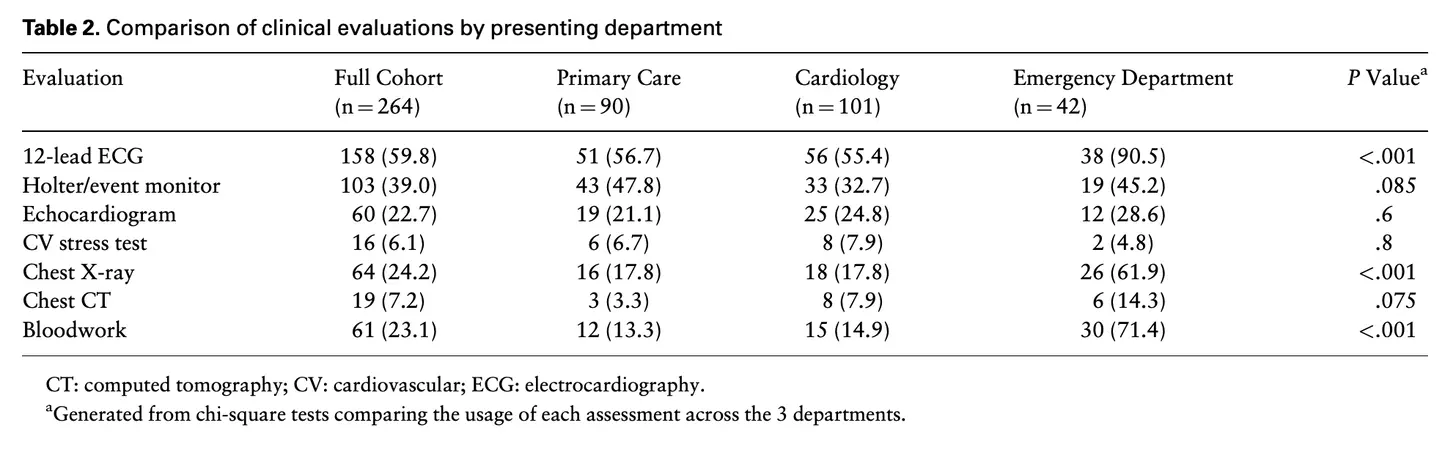
The ECG in the Apple Watch is a good example. Even a few percentage points off in sensitivity of a heart issue will result in millions of potential false-positives that might send people to the hospital out of worry. A small study out of Mayo Clinic suggests this might already happening:
Among 264 included patients, clinical documentation for 41 (15.5%) explicitly noted an abnormal pulse alert. Preexisting atrial fibrillation was noted in 58 (22.0%). Most commonly performed testing included 12-lead echocardiography (n = 158; 59.8%), Holter monitor (n = 77; 29.2%), and chest x-ray (n = 64; 24.2%). A clinically actionable cardiovascular diagnosis of interest was established in only 30 (11.4%) patients, including 6 of 41 (15%) patients who received an explicit alert.
[So in this study only 15% of people that got the alert actually had a clinically relevant cardiovascular issue.]
Some people would see this and say the Apple Watch is going to cause unnecessary strain on the healthcare system. Another way to see it is the Apple Watch is creating a new opportunity for a level of triaging between a home diagnostic and a full blown hospital visit. This is where I think pharmacies can shift their role - becoming a hub to do follow-on testing with higher specificity tests.
In the Apple Watch study, here is a list of follow-up tests done to confirm a cardiovascular issue. I wonder if all of these can be done in a pharmacy with the right tools. Rather than require a referral, the software can immediately escalate at-risk patients to a cardiologist for a remote consult (similar to what Viz.ai has done with the workflows of primary stroke centers). And if a patient needs meds, well, they’re in the right place! This would turn pharmacies into actual places of diagnosis - separating the person collecting the data (pharmacist) and the person interpreting the data (physician).
I think pharmacies can position themselves as escalation hubs, especially as home diagnostics and virtual care become more prevalent and the scope of practice expands for pharmacists. At a certain point of a virtual visit you’ll need certain confirmatory tests you can’t do at home or need a trained clinical staff to perform. Properly staffed pharmacies can be a more cost-effective “first escalation step” for people that are wondering if what they have is serious. This will be even more true as the tools in hospitals see miniaturized, point-of-care versions that can come to the pharmacy like ultrasounds, MRIs, and more.
These would require totally new patient outreach and escalation workflows, and you know how I feel about a good, novel tech-enabled workflow.
Conclusion and parting thoughts
The future of retail and community pharmacies will probably end up splitting the dispensing of goods and the administration of services into two very different business types that build their workflows, operating model, and real estate around one or the other. Right now it’s a weird mish-mash of all of the above.

It’s an exciting moment in healthcare to rethink the roles community pharmacies and pharmacists play - I’m here for it. The only way we’re going to lower the cost of care is by making care more physically accessible, increasing touch points with patients, and triaging care to the most cost-effective form of labor.
Thinkboi out,
Nikhil aka. “I kind of wish pharmacies still sold those cool fountain drinks”
Twitter: @nikillinit
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







