More (GPTish) healthcare startup ideas
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
Last newsletter I asked you all to submit your startup ideas after giving you some of mine. And you didn’t disappoint. There were so many good responses that I felt bad only doing 3, so I added a bunch below with some memes + notes from me.
Using HealtheGPT for data standard transformations
“The goal here is to make patient clinical data portable.
Step 1: Import all patient health system electronic health record (EHR) clinical data into HealtheGPT.
Step 2: interact with HealtheGPT to understand how many unique patients there are and what clinical data objects exist (e.g. demographics, insurance, medications, allergies, problems, immunizations, lab results).
Step 3: Export all the clinical data into a desired healthcare information standard interoperability message format (HL7, FHIR, etc.). HealtheGPT will write the programming code that will translate the raw clinical data into the desired output.
You now have a robust set of portable data to import to any other system in the world. And the process took an hour as opposed to 6-12 months of typical traditional work across dozens of teams. “
-Anonymous (though reach out if you want to work with this person)
[NK note: This raises an interesting question about the role of standards in the future if it becomes super easy to transform any data format from one standard to another nearly instantly. Wait, is that an interesting question? I only talk to people on the internet nowadays
A lot of private enterprises that maintain standards + consulting shops that do these conversions might be sweating a little bit]

Dynamic training for residents
"Basically take cases residents treated from the EHR and allow GPT to help them analyze it after the fact. Go through the whole patient journey, look at the decisions, outcomes, compare to historical data and other cases. It’s personalized for the residents allowing them to learn better from their mistakes + provides feedback for the attending physician about what knowledge gaps need to be filled.
What should it do?
1. Pull from the EHR the cases that the residents treated.
2. Show the residents the whole patient's journey (both in/out of hospital).
3. Let them analyze the decisions made, the outcomes achieved, and how it is compared to historical data and to other cases.
Why is it needed?
* Allows residents to learn from real life cases, and their own experience and mistakes.
* Allows the attending physician to know what are the knowledge gaps that need to be filled, and better understand the learning progress of the residents."
-Boris Goldin (Twitter, Linkedin)
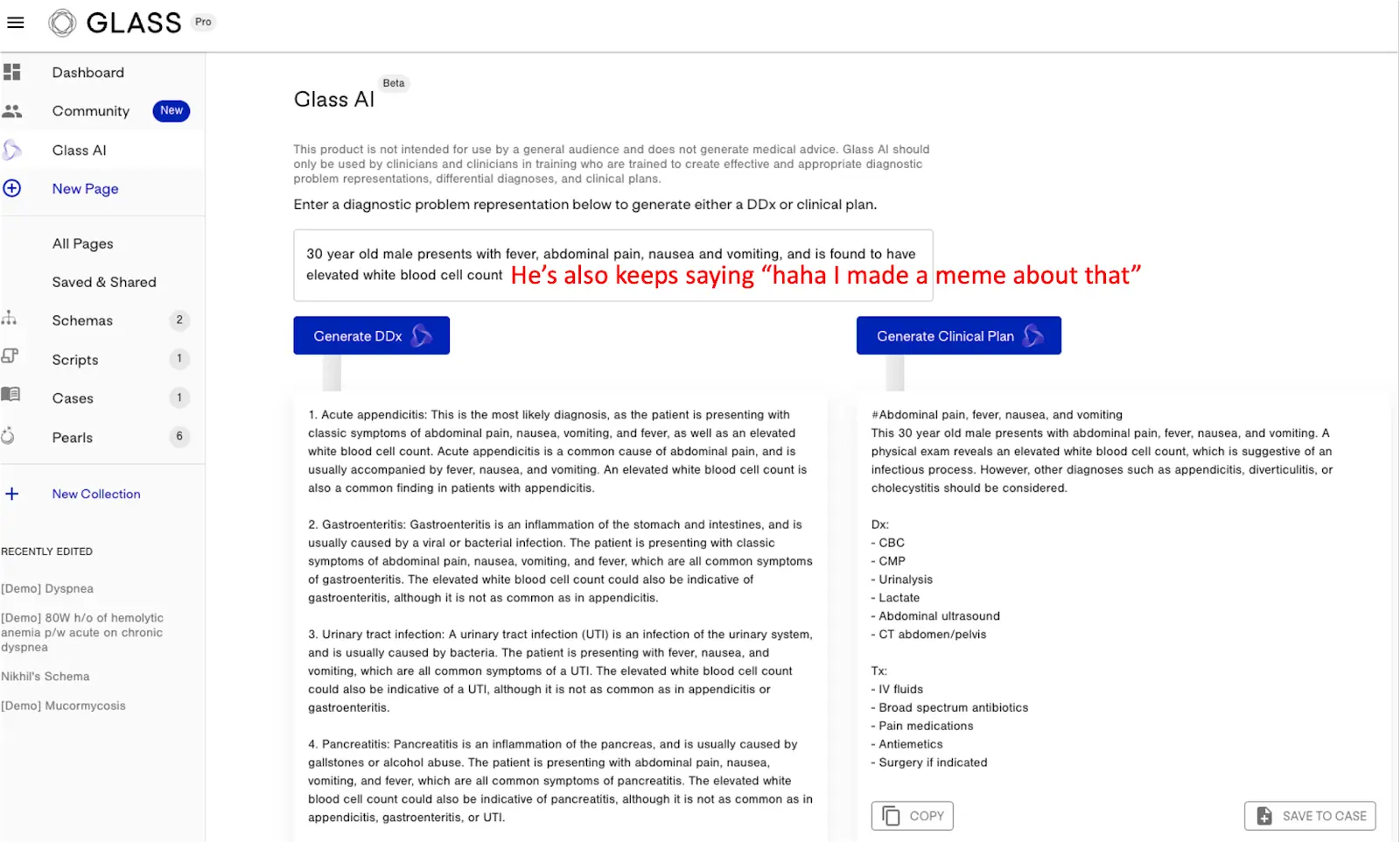
[NK note: Learning and personalized tutoring generally seems like a great use case for large language models, but also requires a high level of accuracy in the answers otherwise you’re teaching wrong information. I’m an investor in Glass, a notebook for doctors that does some interesting stuff using large language models that lets you input a sample patient and how you should think about thinking through a diagnosis/creating a care plan.]
AI Empowered Evidence-Based Guidelines
"The National Comprehensive Cancer Network (aka the NCCN) is a not-for-profit alliance of 32 leading cancer centers devoted to patient care, research, and education. The NCCN develops guidelines for prevention, treatment and management of cancer. Basically they provide clinicians with the “standard of care” of how to best navigate cancer, and the evidence based protocols they develop are essential to the healthcare system. And what’s interesting is that unlike fancy tech companies, they transparently publish their algorithms so people aren’t trying to use them in a black box. This also allows third party experts to help improve them. Imagine that. The problem is that these algorithms and guidelines are published in a PDF (snapshot below) that almost no human can easily process or keep up with, especially given they are frequently updated. So while it may be almost impossible for even a superhuman oncologist to keep up with the NCCN Guidelines…their handy AI assistant might be able to. That’s where OncoGPT comes in.
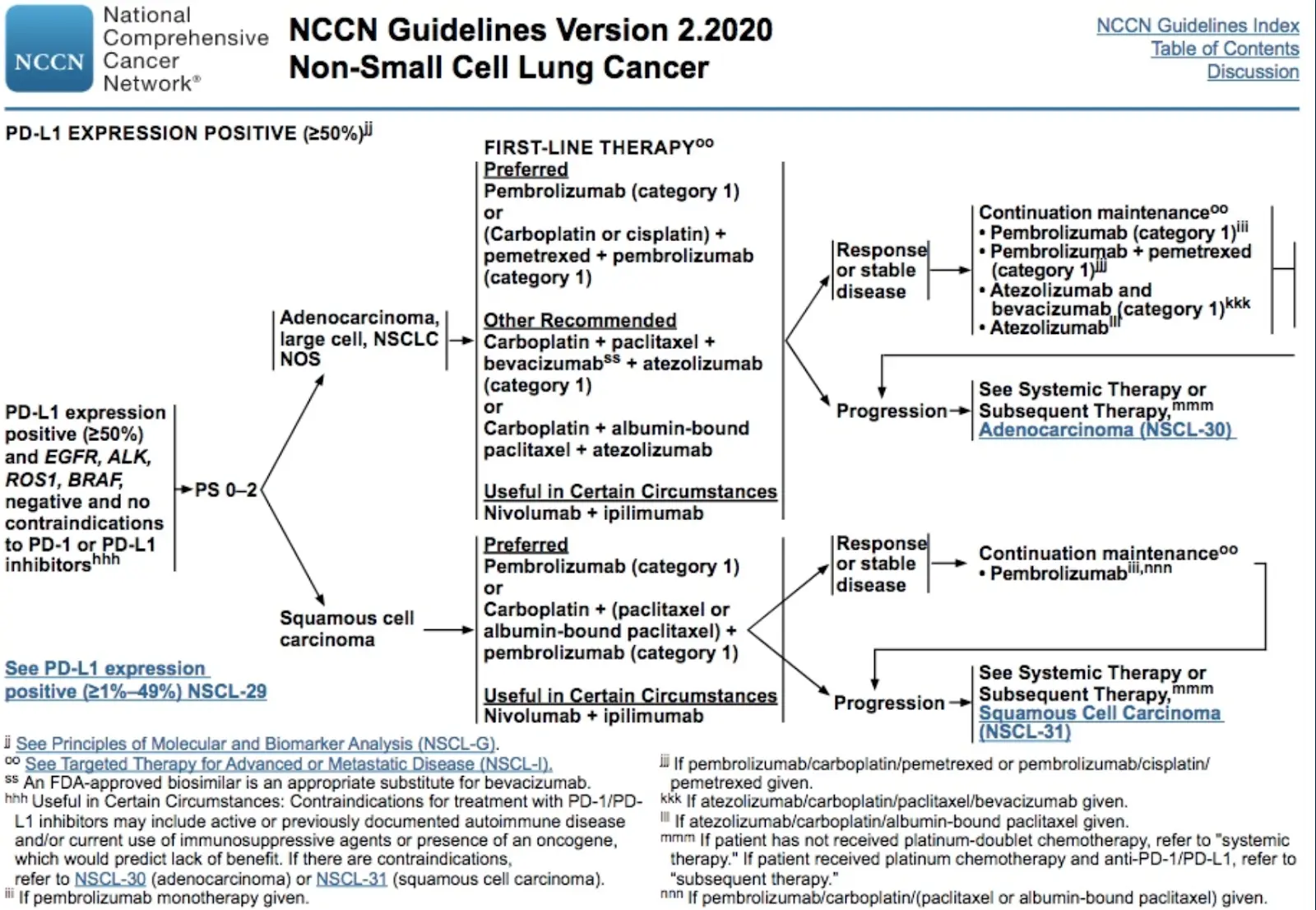
OncoGPT ingests evidence-based guidelines like the NCCN’s, and allows healthcare professionals to easily query the most current recommendations in cancer care. Instead of spending time trying to understand complex maps printed many moons ago, they can just ask. And when these maps change, which they often do, OncoGPT can reconcile and summarize these changes. Healthcare systems will pay for this because it will make physicians more efficient and improve outcomes. OncoGPT can also help empower patients to better understand the options and recommendations being made to them, as they are typically operating in a black box as well. Last but not least, the revenue generated from OncoGPT will be shared with the NCCN and other research organizations that contribute data. More funding = more research = better patient outcomes. See, healthcare becomes really simple with robots.
- David Fisch, Startup Builder & Investor; Passionate about crushing cancer and other diseases
Captain Obvious Disclaimer: biology is really frick’in complicated, and navigating cancer often is too. Even when a patient is fortunate enough to be treated on an existing protocol (some are not, unfortunately), the expertise of a human is still essential. OncoGPT will serve as a technology tool to help physicians and patients keep up with the increasingly rapid pace of innovation in science & medicine, so people receive the best standard of care.
p.s. I really tried to channel my inner Nikhil in writing this. Which means I grossly oversimplified this concept, and I apologize in advance for this. :-\ Especially to the NCCN, which is an organization that I respect immensely."
[NK note: One day “channeling your inner Nikhil” will mean cooler than breaking down evidence-based guidelines. But today is not that day.
I wonder if the concept of generalized guidelines becomes obsolete once we get real interoperability. Instead of general guidelines, physicians will look at patient cohorts like you and see the treatment path that makes the most sense based on historical cases similar to you. Companies like Atropos seem to be trying this in areas like oncology.]
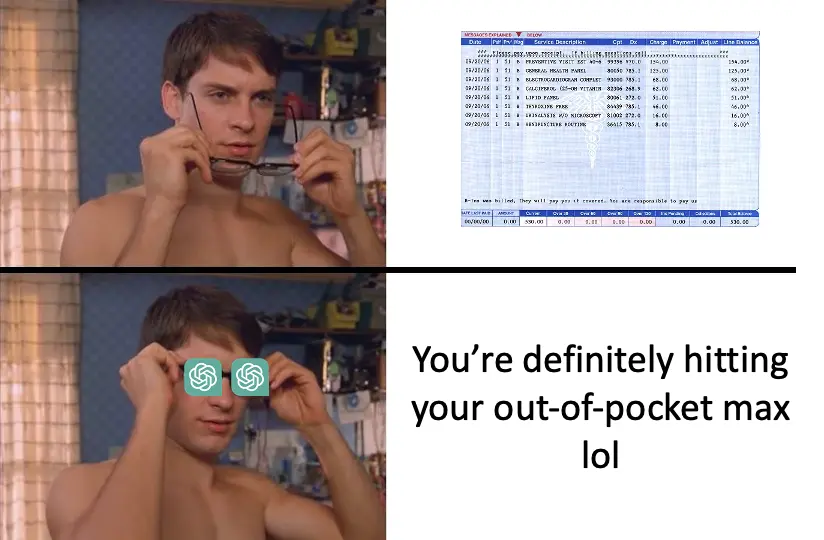
Breaking down the bills
"Okay this is patient facing -- there are a lot of uses for GPT for providers/coders/billers/payers, but I think an LLM is tailor made for breaking down the complicated administrative burden of healthcare bills, payments and appeals for patients.
How I thought of this: My dad got some dental services done ahead of radiation for throat cancer that he had. The bill was around $1800 out of pocket (see what I did there). After calling the billing office once a day from Thanksgiving to Mid-December, the dentist -at a prominent UC medical center tied to his oncologist- said that they never bill Medicare, and any payment of services from Medicare would have to come from us sending the bill to Medicare and getting reimbursed.
I work in underpayment recovery so I knew where to search for the CMS forms, and how to find the right process for it. After I got done rounding up the right documents, I had them ready to send. As a goof, I booted up ChatGPT and gave it the information above, and asked what to do. It was just about dead right on the six or seven steps we had to go through to submit the bill and get reimbursed.
So, my Health-GPT idea is a chatbot that can evaluate bills and patient liability, and give patients the right information and steps to complete so they are not stuck with a bill because of the administrative burden and the complexity of post service payments."
-Tom Nork
[NK note: Something tells me that as soon as patients find a way to make bills decipherable, hospitals will find new ways to make them insane. Like a very mundane arms race.]
Streamline REMS [Risk Evaluation and Mitigation Strategies]
[NK note: REMS are programs that the FDA is essentially requires for drugs that have strong side effects or safety issues like making sure the clinic is equipped to dispense it, monitor the patient, etc.]
"Each REMs program is unique. But I'll give an example below. The main theme is that the requirements for REMS programs made by the FDA are sound and justifiable, but technology has lagged behind making meeting these requirements a seamless experience for consumers. And if the FDA approves a drug and requires a REMS program it's because the drug is so effective it needs to be on the market despite the serious risk which warrants the REMS program or b/c the drug is addressing a seriously unmet need.
Exhibit A is Oral isotretinoin which is curative for severe acne. The drug causes severe birth defects so the FDA understandably has a Risk Evaluation and Mitigation Strategy program in place called iPLEDGE which is a website meant to create a verifiable link between negative pregnancy test and dispensing of the drug in patients that can become pregnant.
Males treated with the drug must manually log onto the site every month to confirm use of a birth control method (usually just by confirming use of condoms if sexually active).
Females on the drug must confirm the use of two birth control methods and have a negative pregnancy blood test each month prior to being dispensed the drug. iPledge website is sucky and labs have to get reordered every month and results manually read and entered into the site by the doc prescribing the drug.
Females on this drug do a ton of waiting. First they wait to see their doctor to see how their acne is improving, then they wait for their doc to order the lab test, then they goto quest and wait to have their blood drawn. Then they go home and wait for their doc to get the results entered (maybe they even have to call to remind them to enter the results), then they go wait at the pharmacy to pick up the prescription. Finally they leave with a drug that cures their acne. Repeat this every month for 6 months which is the usual treatment duration.
There are similar situations/challenges with other REMS drugs.
There's an opportunity for technology to address these challenges and make meeting these requirements an easier experience for docs and patients. In the above example, simply have the data feedback automatically and electronically to the REMS website. Instead this process relies on human entry. Results from most laboratories get uploaded somewhere electronically anyways, so Docs may literally have to login into one website to read the results and transcribe the results into the ipledge website. Ipledge could use a mobile app to send push notifications to males on the drug every month to have them confirm use of condoms instead of making them use a website that may have been built in 1995. Telemedicine and remote patient monitoring are big advancements that could cause disruption in this space too. Patients shouldn't have to wait for their docs to order a lab test to receive their medication when there are solutions like PWN health which are essentially doc ordered lab tests for hire."
[NK note: Using that iPledge website itself is a serious side effect, jesus. A million people have tried building a new electronic patient reported outcomes tool to no avail. Maybe this is a wedge they should explore.]
GoodRx for labs or imaging
"My start-up idea is to one day be able to pull up an app and type in a lab test or imaging study and the patient's insurance/self-pay and out comes a list of locations with estimated prices. As a clinician, I used to have no idea what drugs cost especially in comparison to one another but now I use GoodRx to quickly pull up my planned prescription to get a ballpark estimate.
ChatGPT wrote this as my first slide of my pitchdeck: "Revolutionize healthcare cost transparency with our cutting-edge app! Imagine having the power to easily compare prices for lab tests and imaging studies at the touch of a button. With our app, you'll have access to a comprehensive list of locations and estimated prices, making it easier than ever to make informed decisions about your healthcare. We're taking the guesswork out of healthcare costs, just like GoodRx did for prescription drugs. Get ready to take control of your healthcare expenses with [Start-Up Name]!""
[NK note: I’m actually kind of surprised this doesn’t exist? Medmo can do this for imaging, Labcorp has on-demand, but they don’t seem to have that same awareness or easy to use tools for providers that GoodRx has. Then again, I wish I also didn’t have the awareness of GoodRx.]

The referral report for specialists
"I’ve long dreamed of a GPT-like product that synthesizes clinical information attached to specialist referrals.
First, this would help determine the most appropriate type of care. For example, are our services suitable for this patient? If so, what kind of “visit”? In-person or virtual? At what location? With which possible clinicians? Do they need concurrent tests? Etc, etc.
Second, a specialty-specific summary would enable the specialist to quickly get up to speed before seeing the patient. (The day before my clinics, I routinely spend 1-2 hours sifting through records)."
[NK note: Each doc has their own style of doing this kind of review, it would be interesting if you could tune your summarizer to the information you personally deem important. But what happens if docs default to their summarizer to read through all those pages and the summarizer misses something important? Would malpractice risk scare docs away from doing that?]
Making the most of records - the good, the bad, the RAF
"chatGPT / LLM has tremendous possibilities. While I haven't thought through them as businesses, 3 use cases have come to mind since reading more about it.
1) Synthesizing outside records -- Huge pain point for clinicians (particularly hospitalists and any specialist that has to do 'chart biopsy') when trying to familiarize yourself with new patient. Today, patient or outside facility faxes reams of records with some useful information (cath report or transfer meds for example) to low-value documents. Current state - someone has to flip through these pages of material to glean valuable info. If a chatGPT-type program could sift through the hundreds of pages of unstructured notes and summarize the highest value findings, this would be quite valuable. Could really apply for helping synthesize any pre-visit summary in the future too where outside records are involved, prep the note, etc.
2) Personal Health Record Organization -- Similar concept to above but empowers the patient rather than waiting for the doctor/health system to do it for you. Concept being any after visit summary, test result, progress note, etc can be emailed or faxed to your personal email or fax # and the primary data is stored and chatGPT synthesizes into summarized coherent format for patient to either use for their own knowledge or share with their next care provider etc. Almost like expensify on steroids for your personal med records
3) New way for CMS to do risk adjustment -- This is probably my pie in the sky one but CMS moves away from legacy HCC model and what ICD codes are submitted on a claims file to set RAF, and instead, move to chatGPT like software analyzing entire cohort of claims + available clinical data generated on covered lives to create a more automated and passive way to answer the holy grail question of 'How sick is my patient(s)?' Using ChatGPT to normalize risk adjustment using passive clinical data would likely lead to more accurate risk adjustment but also eliminate the cottage industry of RAF optimization which provides little to no actual patient / clinical value."
-Anonymous medical director
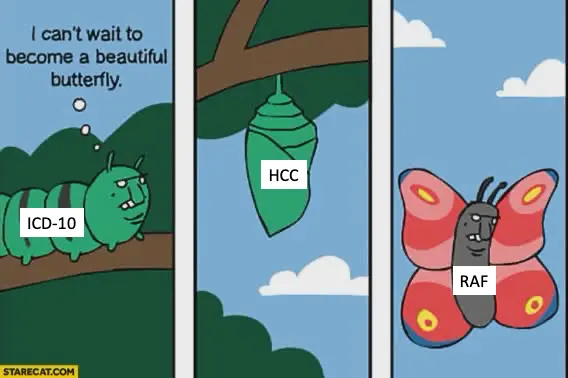
[NK note: As more data starts becoming easier to pull and in the hands of patients/third-parties thanks to the interoperability rules rolling out, we’re going to have more data than we know what to do with (including lots of free text in the records). Applying large language models to interpreting that data and then repurposing it for different end use cases (like the examples above) seem great. But I wonder what happens when you’re depending on AI with variable output to make a somewhat subjective choice of “how sick is my patient panel?”. At least the ICD, HCC, RAF stuff is standardized and auditable.
P.S. We actually go through what an ICD code is, the purpose of risk adjustment, and how RAF works at a high level in the healthcare 101 class, so sign up :).
Thinkboi out,
Nikhil aka. “Snark Tank”
Twitter: @nikillinit
Other posts: outofpocket.health/posts
Featured Jobs
Sign up for the featured tier in the Talent Collective to get your jobs in the newsletter, on Twitter, etc.
- SWORD Health is a digital musculoskeletal therapy provider that pairs its members with a licensed physical therapist. They're hiring a Senior Data Scientist.
- Nimbus Health is building a network of technology enabled pulmonary clinics to address the unmet needs of millions of lung disease patients across America. They’re hiring a Senior Product Manager.
- Taro Health is restoring the doctor-patient relationship as a doctor-powered health insurance company. They’re hiring a Product Engineer.
{{sub-form}}
---
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







