Mental Health And The Weird Fixation With Employers
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveHealthcare 101 Crash Course
%2520(1).gif)
Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
The shift during COVID
Mental health has seen some extreme changes during COVID. Specifically, we saw:
- A full transformation to telemedicine based care for behavioral and mental health even post-quarantine
- The suspension of Ryan-Haight laws
- A massive increase in demand for mental health services exacerbated by COVID and seeing all of your friends get engaged or have kids
- A clear lack of supply of mental health practitioners to meet that demand

During this time, employers in particular became much more fixated on their mental health benefits due to a combination of burnout + staff shortages + intense recruiting/retention of employees.
In response, a ton of money has entered the mental health space, specifically helping employers offer benefits to their employees. However, I personally don’t like this trend and I’ll explain why.
What are Employee Assistance Programs?
It’s worth starting this by explaining how Employee Assistance Programs (EAPs) work. EAPs are voluntary workplace programs that assist employees dealing with mental/behavioral health, general health issues, or anything else in their lives that might be affecting work performance (e.g. grief, legal issues, developed complexes from being told you were gifted growing up but then looking around and wondering if you’re living up to that potential, etc.). About 80% of employers offer an EAP, according to this employee benefits survey.
EAPs largely started and became popular in the 1940s as an occupational alcoholism program that utilized many concepts from alcoholics anonymous. Over time they expanded to increasingly more mental/behavioral health issues and eventually amorphously covered all issues that contributed to absenteeism and workplace productivity.
EAPs offer a variety of services depending where you are, but the “standard” seems to be:
- Free and confidential assessments, short-term counseling (3-5 free therapy sessions), referrals, and follow-up services to employees who have personal and/or work-related problems
- Crisis intervention services available 24 hours a day, days a week, including critical incident support like offering on-site counseling after a death in the workplace
- Procedures for determining when to provide short-term problem-resolution services within the EAP and when to refer a client to professional or community resources outside the EAP
- Training for the employer’s leaders, so leadership learns to recognize issues and can intervene by referring employees to the EAP
There are lots of customizations to specific employers beyond this. Starbucks offers childcare matching, eldercare matching, financial consultations, and legal consultations, for example. Some companies offer mindfulness and breathing exercises (useful if you need to tell employees your company is switching to Microsoft Teams). While many companies used to manage these programs themselves and staff them accordingly, over the last couple of decades, it’s largely become something that’s been outsourced to external third-parties.
EAPs have several different types of pricing. One is per member per month. The more per month you pay, the richer the plan is and might include more therapy sessions per patient or other benefits. Another is per visit pricing when employees utilize the services. Most companies tend to use a hybrid of the two. You can see below an example where there’s PEPM pricing + fee-for-service for the extras.

The Mental Health <> Employer Conundrum
In the last few years, a lot of mental health companies set their eyes on the EAP segment as a potential sales channel or even to rip and replace them completely. During COVID, mental health benefits have become a key pillar in employee retention/attraction and addressing absenteeism.
However, I think there are a few structural problems with the employer channel in healthcare which is why I’m not really a huge fan of companies that go down this route.
I beat this drum all the time, but the principal-agent problem once again rears its head when the buyer (employer) cares about something different (price) than the user (patient, who cares about experience + feeling better). This is why EAPs have essentially become a race to the bottom on pricing, where some carriers even offer it for “free” bundled with the other core insurance products. However in order to make the economics work on increasingly cheaper plans the quality of the product itself has gotten way worse and in the worst cases the parts of pricing that are flat fees actually disincentivizes employees from using the EAP itself.

Perhaps relatedly, utilization for EAPs is comically low. Most benchmarks put it around ~5%, though friends of mine that are closer to these numbers say it’s way lower than that. There aren’t even actual standards around utilization. Some companies will consider talking with a therapist as utilization but some companies that include digital CBT and content (which have lower wait times and less friction) will include those as utilizing services so they can seem much higher. But if you talk to anyone involved in purchasing or administering these programs, they know the utilization is dogshit. Some EAPs are now making performance guarantees around utilization, but again they’re choosing utilization metrics in most of those cases.
Though pricing might be one reason, the other reason could also just be the crazy idea that workplaces which are in control of your employment may not be the place people feel encouraged to access mental health services! This is especially true if managers and bosses are not actively talking about using the services. In a worst case scenario, having your therapist notes potentially subpoenaed because of other things happening at work demonstrates exactly why someone might not use these services (at a time they probably need them most).

We should want health benefits to be portable beyond your employer, and I think this is doubly true for mental health where finding an effective therapist that works for you can be a struggle. Losing access to someone you work well with just because you leave a job shouldn’t be a system we want.
Do Employers Shift Clinicians To The Wrong Places?
There’s also a larger, societal issue that’s a downstream effect of the employer focused business model for mental health companies.
Currently, there is a clinician shortage for addressing mental health. About 1 in 5 people have some form of mental health disorder which has clearly increased during COVID. Reputable surveys suggest more than 22% of essential workers have contemplated suicide in the last 30 days. Most projections show that across all levels of scope we’re going to have an even worse shortage.
This analysis from HHS/HRSA has different scenarios for number of trainees, amount of utilization + disease prevalence all before COVID.

Because of how much more lucrative the employer channel is while treating generally less acute/complex cases, we are seeing a diversion of our limited clinician supply away from the populations who are at higher risk, have severe mental illness, and generally covered under Medicaid/Medicare.
This is something I’ve heard anecdotally from friends that work in clinician recruiting. Telemedicine for mental health services has become normalized and widespread while burnout is at an all time high for front-line staff dealing with complex mental health patients that need in-person care (who have largely gotten worse during the pandemic). Moving to a cushier desk job for largely low acuity patients and simple cases like low level anxiety/depression has never seemed more attractive.
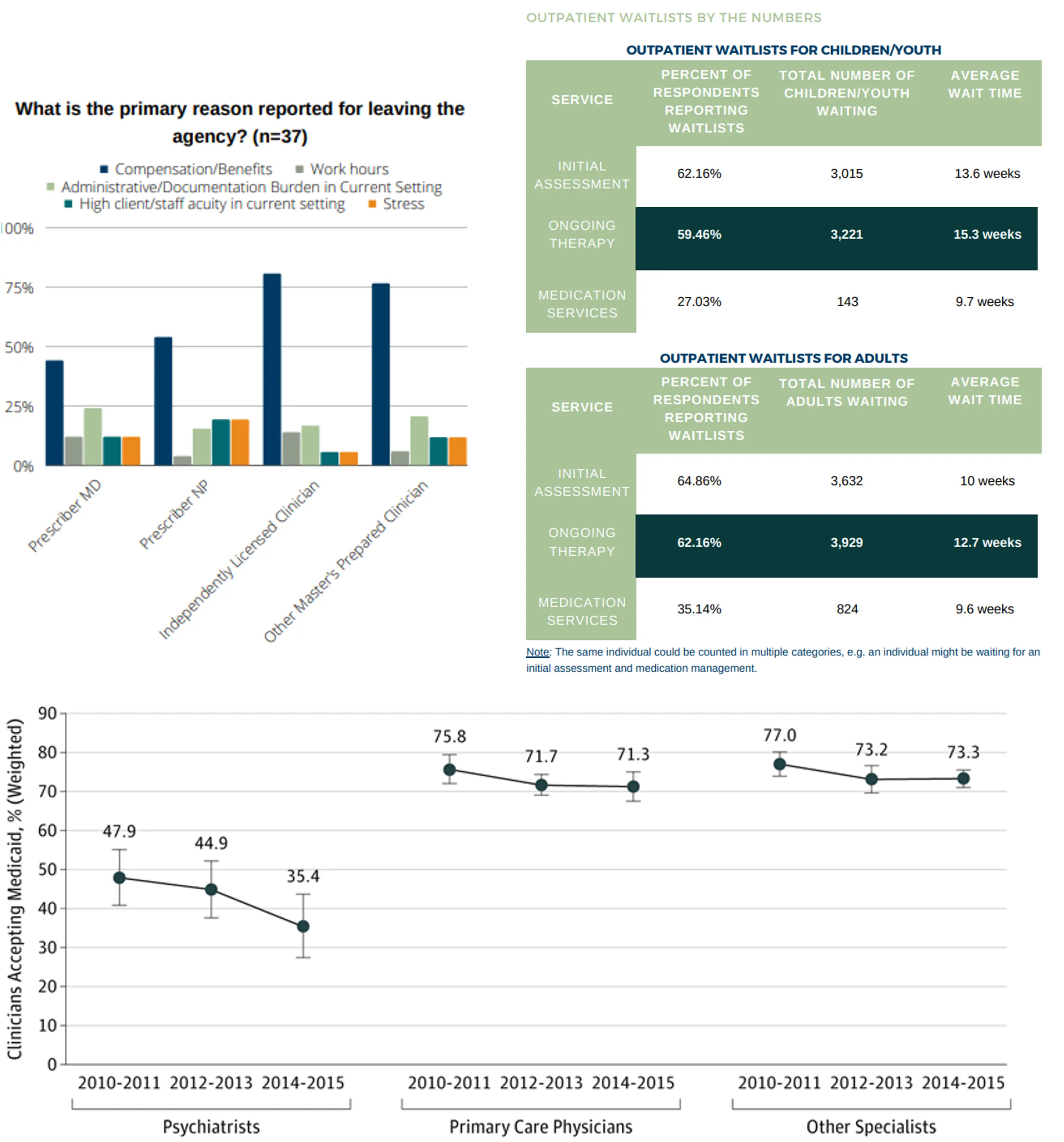
I wish I had more data to substantiate this claim (I was looking into wait times by payer coverage yet couldn’t find much out there.). But it’s not hard to put two and two together: psychiatrists who accept Medicaid are dwindling, trying to find a clinician accepting new patients for complex issues like bipolar disorder is impossible, the waitlists are growing for outpatient mental health centers, and most people leaving these mental health service agencies are due to salary. Yet EAP providers are competing on availability of care quickly. I’ve been told some clinicians make more money in one day working with a tech-enabled EAP provider than four days as a university counselor.
Am I knocking employers for offering these services? Absolutely not - they’re doing what they think is best for employees. But do I think it sucks that one of the most viable mental health business models has inherent structural issues and potentially shifts the limited mental health workforce we have away from the most at-need? Yes.
It's an uncomfortable conversation. We’ve increased demand for therapy services thanks to de-stigmatization + encouraging people to go to therapy without increasing the commensurate supply of clinicians that can address those needs. Combine that with way worse reimbursement for dealing with complex cases and severe mental illnesses getting exacerbated, and the result is maybe directing care away from those who need it most.
Conclusion
For now, most mental health companies seem to focus on new distribution channels, increasing demand for mental health services, and matching between patients and providers in some capacity. Those are less interesting to me because they don’t fix the core issue, supply. We don’t have enough clinicians to address this demand even if we increase it.

Next week I’ll talk about some of the areas I’m more interested in within the mental health space.
Thinkboi out,
Nikhil aka. “men will literally write about therapy instead of going to therapy”
Twitter: @nikillinit
Other posts: outofpocket.health/posts
Thanks to Morgan Cheatham, David Ricupero, Tyler Fasanella, and John Hansbrough for reading drafts of this
{{sub-form}}
---
If you’re enjoying the newsletter, do me a solid and shoot this over to a friend or healthcare slack channel and tell them to sign up. The line between unemployment and founder of a startup is traction and whether your parents believe you have a job.
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.