How should physicians get paid?
Get Out-Of-Pocket in your email
Looking to hire the best talent in healthcare? Check out the OOP Talent Collective - where vetted candidates are looking for their next gig. Learn more here or check it out yourself.
 Hire from the Out-Of-Pocket talent collective
Hire from the Out-Of-Pocket talent collectiveIntro to Revenue Cycle Management: Fundamentals for Digital Health

Featured Jobs
Finance Associate - Spark Advisors
- Spark Advisors helps seniors enroll in Medicare and understand their benefits by monitoring coverage, figuring out the right benefits, and deal with insurance issues. They're hiring a finance associate.
- firsthand is building technology and services to dramatically change the lives of those with serious mental illness who have fallen through the gaps in the safety net. They are hiring a data engineer to build first of its kind infrastructure to empower their peer-led care team.
- J2 Health brings together best in class data and purpose built software to enable healthcare organizations to optimize provider network performance. They're hiring a data scientist.
Looking for a job in health tech? Check out the other awesome healthcare jobs on the job board + give your preferences to get alerted to new postings.
Today I have a new post and discussion question.
To reiterate the rules:
I’ll pose a question and give my thoughts if I have any. In a future newsletter I’ll include ~3 of my favorite answers people reply with. I’ll possibly even make a meme related to your answer.
Good answers are ones with a novel viewpoint, data to back up their claim, personal stories, and avoid clearly shilling something.
Please reply to this email with your thoughts on the question and let me know if you want to have your name or be anonymous. You have to actually be on the newsletter to submit a reply to it obviously.
Try to keep answers to 2 paragraphs or less please. This obviously doesn’t apply to me because it’s my newsletter and these are house rules.
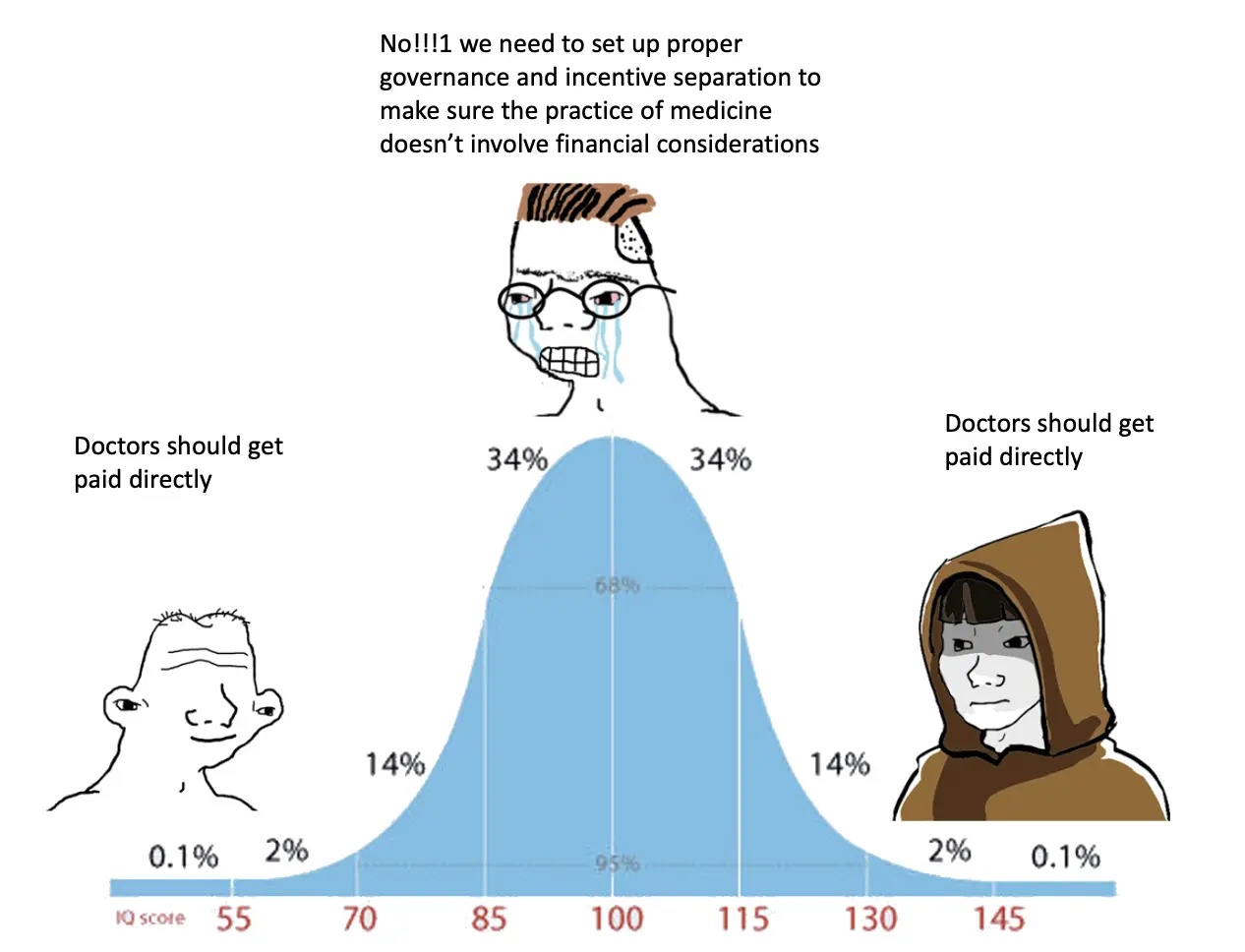
Should we build a system that assumes clinicians are financially motivated?
The US strives to have a system where the care your clinician gives you is divorced from their financial motivation. Should that be what we strive for? Do we currently have that? Here’s a bit on how I’ve been thinking about it (and there are definitely areas I could be wrong here, so hold me accountable/teach me).
Let’s start with whether we have a system that separates a physician’s financial motivations from care delivery. There’s no consistency around the rules in which clinicians receive money and how that affects care.
- Clinicians can’t pay others to give them referrals due to anti-kickback laws. However hospitals can buy primary care groups who “refer internally” to other specialists, imaging centers, labs, etc. So clearly there’s already a warping of referral patterns happening because of financial interest.

- Clinicians do get paid consulting fees from pharma and medical device companies (I wrote a whole thing about this dynamic).
- Clinicians at larger health systems see their compensation tied to Relative Value Units (RVUs), which give higher weights to tests, procedures, etc., so it’s not like the two are completely separate.
- Docs can be large equity owners/founders in companies and run the departments where the trials/pilots are conducted which creates lots of weird and potential conflict of interest issues (see the story of naxitamab for example).
- The Corporate Practice of Medicine (CPOM) doctrine is supposed to prevent corporations/non-clinicians from employing clinicians to prevent care from being influenced. But each state enforces these very differently (and some don’t even have rules around this) which makes it also possible to use telemedicine to arbitrage these rules. Plus, you can get pretty flexible with “Friendly PC” models anyway.
Those are just a few examples, I’m sure there are more. But in general what seems to have happened is that management and administrators are basically controlling who gets financial upside since they have fewer rules around being financially incentivized, and then they place rules on the clinicians who influence how dollars arrive to the health system. Those clinicians will frequently find side avenues of cash for themselves (consulting, etc.) which are usually net benefitting to the hospital as well. It’s hard to claim that we have a system where clinicians aren’t currently influenced by how money is moving, it’s just more indirect.
Basically it seems that in order to get more money as a physician, the goal is to prove your value to the larger hospital. And coincidentally, the hospital basically only cares about optimizing for fee-for-service revenue since that’s where they get all of their money. So if you’re a physician that wants more money, your goal is to help hospitals optimize for the most money.
With fewer and fewer physicians being independent and instead working for some corporate entity, more physicians are now at the whims of the parent company to get that personal financial upside.
Here’s a paper that looked at four high-volume procedures to see what was causing the growth in prices. Turns out that most of the growth is in the facility prices instead of the clinician prices. The hospital keeps consolidating market power, increasing prices via facility fees, and then the hospital system decides where the increase in money goes to.

This is also complicated in value-based care arrangements, where frontline clinicians have to do a ton of the work involved in hitting metrics associated with better outcomes but don’t necessarily get paid more for it. Plus, as we try to move to value-based care arrangements we end up making it much more difficult for small, independent practices to participate because it might trigger anti-kickback stuff if they coordinate care across other doctors (which is why we end up needing to make carve outs).
So in my head we have three ways forward.
The first is we try to keep what we have today - attempts to separate a direct connection between clinicians delivering care and their financial motivations, which gives hospitals more leverage as employers and yields indirect ways that care is optimized around fee-for-service $$. There are probably incremental fixes we can make here but that’s less fun for the purposes of this post.
The second is that clinicians go straight salaried with fixed % increases in each specialty and there are stringent rules/enforced rules around any kind of potential influence on their care. To me this feels impractical and would end up creating walls between clinicians and the rest of the industry when those relationships can actually be very useful (e.g. in drug development). Plus we’d likely lose a lot of great clinicians who feel like they could get paid more in other countries/industries.

The third and maybe more “out there” version is that we let clinicians make money more directly in whichever ways they want, but they have to disclose everything. Another requirement would have to be that you hook your Electronic Medical Record to some form of registry so that any practice patterns detected as egregious or sus would get flagged to an auditing authority. With so much data exhaust and modern analytics you should be able to highlight egregious clinicians.
I genuinely believe that the majority of clinicians care more about good patient outcomes than they care about personal financial compensation, and that the number of people that would grossly take advantage of this system is small. Frankly they’re already probably doing it in the current system shielded behind the veil of the larger hospital name.
The general idea is to set up a system where physicians are still financially motivated, but instead they get more money by appealing to patients and other physicians instead of hospitals that control their wages and bonuses.
If transparency were forced, I think sets of tools would emerge to show patients exactly what their doctor is motivated by + show other doctors how their peers are making money + let payers take that into consideration when designing networks. I think it would yield some combination of social and financial pressure that would keep outlandish behavior mostly in check. If patients saw that clinicians were getting most of their money from value-based care arrangements, would they be more incentivized to go to that clinician vs. one that is almost entirely fee-for-service?
I wonder if a radically transparent but payment permissible system would have some benefits:
- A lot of these back-office workarounds like the “friendly PC” model are really a wild west and seem semi-subject to the ethical compass of company leadership. More transparency might create more clear rules and guardrails for workarounds that are already being implemented today (and might hopefully reduce the legal fees to set these up smfh)
- By forcing the data into the open, it might actually encourage undervalued clinicians to realize they’re being underpaid and bargain accordingly. You can look at companies like Aledade which do this for independent primary care physicians to hit certain metrics to take advantage of value-based care programs like the Medicare Shared Savings Program.
- You could more easily give direct incentives to physicians to participate in value-based care arrangements and get reimbursed more appropriately for the extra work they have to do. If you make it radically transparent you might actually incentivize providers to take money from “good” places and value-based care arrangements directly.
The Sunshine Act is sort of a mixed bag as an example of radical transparency. It required clinicians to disclose industry payments from pharma and med device companies. Total value of payments went down, but average/median payment went up. So the clinicians that were taking small amounts stopped and the outliers became way more apparent/took more money. I’m sort of surprised tooling hasn’t come up to bring that info into applications, but I think if it surfaced this info to patients when they were choosing their clinician the patient would at least be more wary of the outliers.
The other effect is that it made physicians generally more wary of any sort of interaction with pharma, regardless of whether that interaction was positive or suspect. You can interpret that as good or bad.

Another common pushback would be that physicians will then only pick patients that are the most directly lucrative to them, which to be honest is already subtly the case in our current mostly fee-for-service environment. Maybe transparency will push more physicians to go into value-based care arrangements that include risk-adjustment that would pay them more for taking on sicker patients (and would probably cost the system more, but you can’t win ‘em all).
And then there’s the question of who decides which clinician are practicing “badly” even with transparent data. It’s easy for simple cases to figure out if a clinician is going rogue, but for more complex cases there may not be clear guidelines on what to do.
Anyway I don’t even know if I actually believe this system would be better, it’s just a thought experiment. At the very least we should be honest with ourselves that physicians are financially motivated and the current system is inconsistent and restrictive (positively and negatively) in the way physicians can get money.
What do you think a better system would be? Or is the one we have working (maybe with some fixes)?
Thinkboi out,
Nikhil aka. "support your small, local physician paying off their student loans"
Twitter: @nikillinit
Thanks to Dan O’Neill, Gina Siddiqui, and Neil Sanghavi for reading drafts of this
{{sub-form}}
Healthcare 101 Starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 Starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Healthcare 101 starts soon!
See All Courses →Our crash course teaches the basics of US healthcare in a simple to understand and fun way. Understand who the different stakeholders are, how money flows, and trends shaping the industry.Each day we’ll tackle a few different parts of healthcare and walk through how they work with diagrams, case studies, and memes. Lightweight assignments and quizzes afterward will help solidify the material and prompt discussion in the student Slack group.
.png)
Interlude - Our 3 Events + LLMs in healthcare
See All Courses →We have 3 events this fall.
Data Camp sponsorships are already sold out! We have room for a handful of sponsors for our B2B Hackathon & for our OPS Conference both of which already have a full house of attendees.
If you want to connect with a packed, engaged healthcare audience, email sales@outofpocket.health for more details.







